AI blood testing technology can detect lung cancers
Artificial intelligence blood testing technology developed at Johns Hopkins’ Sidney Kimmel Comprehensive Cancer Center has detected over 90% of lung cancers in samples from nearly 800 individuals with and without cancer, according to a new study published in the journal Nature Communications.
Lung cancer is the most common cause of cancer death, claiming almost 2 million lives worldwide each year. However, fewer than 6% of Americans at risk for lung cancers undergo recommended low-dose computed tomography screening, and even fewer are screened worldwide. This is due to reasons including concerns of potential harm from investigation of false positive imaging results, radiation exposure or worries about complications from invasive procedures.
“It is clear that there is an urgent, unmet clinical need for development of alternative, non-invasive approaches to improve cancer screening for high-risk individuals and, ultimately, the general population,” said lead author Dimitrios Mathios, a postdoctoral fellow at the Johns Hopkins Kimmel Cancer Center.
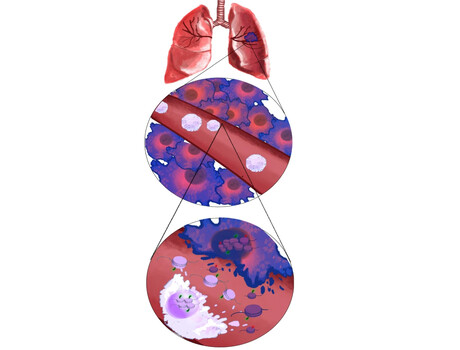
DELFI (DNA evaluation of fragments for early interception) technology uses a blood test to indirectly measure the way DNA is packaged inside the nucleus of a cell by studying the size and amount of cell-free DNA present in the circulation from different regions across the genome. Healthy cells package DNA like a well-organised suitcase, in which different regions of the genome are placed carefully in various compartments. The nuclei of cancer cells, by contrast, are like more disorganised suitcases, with items from across the genome thrown in haphazardly.
When cancer cells die, they release DNA in a chaotic manner into the bloodstream. DELFI helps identify the presence of cancer using machine learning to examine millions of cell-free DNA fragments for abnormal patterns, including the size and amount of DNA in different genomic regions. This approach provides a view of cell-free DNA referred to as the ‘fragmentome’. It also only requires low-coverage sequencing of the genome, enabling this technology to be cost-effective in a screening setting.
Investigators from Johns Hopkins, working with researchers in Denmark and The Netherlands, performed genome sequencing of cell-free DNA in blood samples from 365 individuals participating in a seven-year Danish study called LUCAS. The majority of participants were at high risk for lung cancer and had smoking-related symptoms such as cough or difficulty breathing. The DELFI approach found that patients who were later determined to have cancer had widespread variation in their fragmentome profiles, while patients found not to have cancer had consistent fragmentome profiles.
Subsequently, researchers validated the DELFI technology using a different population of 385 individuals without cancer and 46 individuals with cancer. Overall, the approach detected over 90% of patients with lung cancer, including those with early and advanced stages and with different subtypes.
“DNA fragmentation patterns provide a remarkable fingerprint for early detection of cancer that we believe could be the basis of a widely available liquid biopsy test for patients with lung cancer,” said study author Rob Scharpf, Associate Professor of Oncology at the Johns Hopkins Kimmel Cancer Center.
A clinical trial called DELFI-L101, sponsored by Johns Hopkins University spin-out Delfi Diagnostics, is now evaluating a test based on DELFI technology in 1700 participants in the US, including healthy participants, individuals with lung cancers and individuals with other cancers. The group would like to further study DELFI in other types of cancers.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Blood test could be used to diagnose Parkinson's earlier
Researchers have developed a new method that requires only a blood draw, offering a non-invasive...
Cord blood test could predict a baby's risk of type 2 diabetes
By analysing the DNA in cord blood from babies born to mothers with gestational diabetes,...
DNA analysis device built with a basic 3D printer
The Do-It-Yourself Nucleic Acid Fluorometer, or DIYNAFLUOR, is a portable device that measures...





