Cold plasma boosts the power of antibiotics
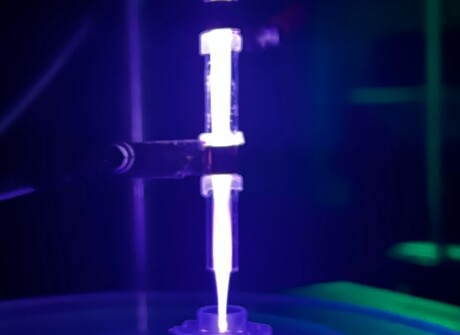
Researchers from Queen’s University Belfast and Thomas Jefferson University have found an innovative way to amplify the power of antibiotics, using cold atmospheric-pressure plasma as a weapon to enhance their strength. This scientific advancement, described in the journal Biofilm, could provide a solution to the global health crisis of antibiotic resistance.
More than five million deaths are attributed every year to antimicrobial resistance, as once easily treatable infections like pneumonia, wound or bloodstream infections are becoming increasingly resistant to existing antibiotics. The researchers discovered that by merging cold plasma and antibiotics, it can significantly weaken Pseudomonas aeruginosa biofilms; a common bacterium that often causes hard-to-treat infections. This new approach makes them significantly more susceptible to treatment.
“Our research demonstrates the immense potential of combining cold plasma with antibiotics in the fight against superbugs,” said lead author Jordanne Maybin, a PhD student at Queen’s University Belfast. “This innovative approach not only offers a more effective treatment option but could extend the useful lifetime of our current antibiotics. It’s a potential breakthrough that could buy time in the race against antibiotic resistance.”
The researchers said their discovery could revolutionise the way bacterial infections, particularly those caused by antibiotic-resistant bacteria, are tackled. By demonstrating the significantly enhanced effectiveness of antibiotics when combined with cold plasma against Pseudomonas aeruginosa biofilms, they have uncovered a promising new avenue in the ongoing fight against deadly superbugs.
“Cold plasmas are a reasonably recent antimicrobial technology and this combination not only offers a potential route to effective management of infections with much lower doses of antibiotics than are normally needed, but also some important observations in how bacteria respond to cold plasma treatment, which will allow us to optimise the technology further,” said principal investigator Professor Brendan Gilmore, who leads the Biofilm Research Group at Queen’s University Belfast.
Envisioning the future, the researchers anticipate infections becoming less severe, treatment times reducing and infection occurrences dropping. Their work not only aims to enhance present treatment methodologies but also seeks to inspire novel strategies to tackle antibiotic resistance.
“Our research has given us an edge,” said study co-author Dr Thomas Thompson, a Research Fellow at Queen’s University Belfast. “It’s providing a well-needed turbo-boost to our antibiotics — a crucial step in confronting global health threats like antibiotic resistance.”
Biomarkers for SIDS found in blood samples
US researchers have revealed the fingerprints of sudden infant death syndrome (SIDS) within blood...
Uncurling and 'gluing down' DNA molecules for sharper imaging
Researchers at Nagoya University have demonstrated techniques for stretching and immobilising DNA...
Novel 3D bioprinter can replicate human tissue
Biomedical engineers have invented a 3D printing system capable of fabricating structures that...




