Adopting immunity
Drs Leighton Clancy and Emily Blyth are developing and conducting clinical trials on virus-specific and tumour-specific T cells with the ultimate goal of producing an improved treatment package for bone marrow transplant patients.
Bone marrow transplant is a successful treatment option for patients with cancers of the blood, bone marrow and lymph nodes. The use of allogeneic transplants, where bone marrow or bone marrow stem cells are donated from another person, has become one of the best ways to treat patients for diseases such as lymphoma and leukaemia.
But even though a transplant may cure a patient of their disease, their resultant poor immune function can lead to them dying from infection. In fact, one of the major morbidities within the first 12 months after a bone marrow transplant is infection.
Tackling this morbidity rate provides the main driving force for Dr Emily Blyth, clinical physician at Westmead Hospital in Sydney, and senior hospital scientist Dr Leighton Clancy, whose work began with making viral-specific T cells.
A clinical need
Patients undergoing blood and marrow stem cell transplants first undergo chemotherapy to wipe out their diseased marrow. They are then given a bone marrow transplant to replace their diseased tissue with healthy tissue.
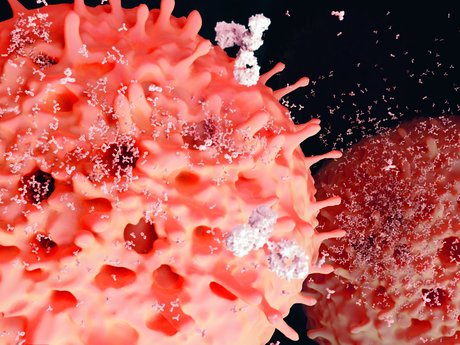
A major side effect of this process is that the patient’s T cells are wiped out - the CD4 and CD8 T cells - which play a central role in cell-mediated immunity against pathogens such as viruses.
T cell recovery tends to be slow after transplant. It can take 12 months to 2 years in children and even longer in adults because of their less efficient thymus - the educational centre for generating new T cells. And without functional T cells, patients are susceptible to infection.
The big three
Infection with cytomegalovirus (CMV), Epstein Barr virus (EBV) and adenovirus is particularly frequent amongst bone marrow transplant recipients. These are the big three and they are often used as prognostic markers after transplant.
CMV is a common virus that is usually without symptoms in healthy people.
“This is one of the most important viruses after transplant because about half of patients have been infected and in that group going into transplant a large proportion of them - up to 70% - get CMV problems after transplant,” said Blyth.
CMV is a herpes viruses, like EBV. Herpes viruses can lie dormant within cells in the body and reactivate when the immune system is compromised. In the absence of T cells, as in transplant patients, these viruses can emerge or reactivate, causing problems that can be fatal.
EBV is less common than CMV but more fatal, reactivating to cause new B cell lymphomas.
“The case fatality rate of EBV tumours after transplant is quite high,” said Blyth. “It’s quite devastating, you are cured of your original illness and you die of a new cancer that’s caused by the immune deficiency of your transplant.”
Viral screening and antiviral treatments can help to reduce these complications, but the treatments are not always effective and have their own risks. As Blyth explained, some antiviral drugs, in particular those used to treat CMV, cause bone marrow suppression or kidney problems.
Virus-specific T cells
The first clinical trial the researchers conducted was with T cells specific to CMV, EBV and adenovirus. This involved 50 patients and ran from 2003 to 2013.
The work was published in the journal Blood in early 2013 and is the biggest adoptive immunity study against CMV conducted in the world to date.
The results were promising. Patients given viral-specific T cells post-transplant were found not to get sicker when compared to patients not given treatment, demonstrating safety for the procedure.
The study also showed that patients who had CMV increased their CMV immunity; that is, their T cells expanded and proliferated, functioning in a normal way to provide immune protection to the patients.
Another finding was that patients who did develop CMV reactivation had quite low levels of reactivation. This implied that the T cells were effectively preventing infection, which in turn meant that patients needed less antiviral treatment.
“Patients who undergo CMV reactivation after transplant go onto an automatic antiviral treatment process and they keep receiving this treatment until the problem is solved,” Blyth explained. “Our patients had lower CMV reactivation because of the T cell treatment, so they stopped antiviral treatment more quickly and used half as much drug than those patients who did not receive T cells.”
This, in turn, meant they also suffered fewer side effects and complications and had a better quality of life. Not to mention the lower healthcare costs.
“Antiviral treatment can cost $15,000 per course in someone with multiple CMV problems. If we can tweak the infusion process and improve it we could potentially get better outcomes than in that study,” Blyth predicted, adding that they plan to look at health economics and conduct randomised studies in the next phase of studies.
Refining the process
At that stage the researchers were using T cells isolated from the blood of donors.
This involved collecting blood from donors and processing it to obtain T cells and the potent antigen-presenting dendritic cells. Using an adenoviral vector, genes coding for CMV antigens were delivered to the dendritic cells, which were then mixed with T cells from the donor activating them to recognise the CMV antigen. The T cells were then grown in culture for about three weeks to generate sufficient cells to give to patients.
“Much of my work has been about trying to make this process more efficient,” said Clancy. “Although we have used the adenovirus vector for the majority of patients, more recently we have switched to using overlapping peptides corresponding to CMV, or other viral antigens. This was to improve efficiency, reduce cost, improve safety, etc. For this technique to become routine and cost effective, it’s important to find ways of making the process more efficient.”
And Clancy has done just that. Another improvement that revealed itself to him during the long hours in the lab was to source the T cells from the donor’s stem cell harvest, rather than taking an extra blood sample.
“It struck me that we could use the stem cell harvest that had already been collected as the source of T cells, otherwise we are duplicating everything in our process,” Clancy recalled. “And we only use a tiny proportion (<1%) of the stem cell harvest to manufacture the virus-specific T cells. This overcomes some of the logistics such as getting blood from donors who live overseas, from whom a separate collection is impossible."
It also avoids duplication of donor assessment, infectious disease testing, blood collection and transport.
About half the unrelated bone marrow transplants in Australia come from donors located overseas. This makes it highly unlikely that a blood sample could be later obtained from these donors to generate T cells.
“The important thing in terms of impact for patients is that it’s increased the number of patients that could potentially have this treatment by double just with this one innovation,” Clancy added.
Once they demonstrated that antiviral T cells with the same specificity and efficacy could be created directly from the stem cell harvest, the work shifted to follow this course.
An immune system transplant
With promising results under their belt and a refined technique, the researchers then started looking at creating virus-specific T cells for other infections.
Transplant patients are susceptible to many infections - a simple flu virus, for example, can kill a patient post-transplant because of their low immunity.
The researchers have developed methods to isolate the T cells for about seven different pathogens, including the flu, chicken pox (varicella), BK virus, the fungal Aspergillus species as well as other fungal infections.
“We thought the best way of approaching this would be to reconstitute a patient’s immunity before they develop problems,” said Blyth.
Developing a type of routine early transplant preventative therapy for patients is in the preclinical phase with a small pilot study underway involving 10 patients using different multivirus T cells.
“This is the first trial with this many pathogens being targeted at the one time,” said Clancy. “We are giving patients about seven different multivirus T cells.”
The ultimate aim is to confer as close to normal immunity possible to bone marrow transplant patients.
A T cell bank
Another project the researchers are working on is creating a T cell bank. This would supply off-the-shelf T cells allowing each patient to be given the specific mix of T cells they need.
“The aim is to produce a bank of donor T cells of common HLA type, grow up large numbers of these, aliquot them and freeze them for later use,” explained Clancy. “The idea is to have a bank of antiviral cells ready to go for people who need them immediately and you could search for the most closely HLA-matched product and choose this for a particular patient.”
Matching tissue types involves matching the human leukocyte antigen (HLA) and usually involves a family member, but if no family member is available, a search is made to find a suitably matched unrelated donor.
There are six main HLA loci encoding for the HLA antigens that are presented on the surface of almost all nucleated cells. They are important molecules in tissue recognition and matching HLA loci is crucial in stem cell transplants because HLA mismatching can initiate rejection of a graft or the development of graft versus host disease.
In initial studies the T cell products were HLA-matched between donors and recipients at five or six alleles, which is close to fully matched.
Now, the researchers are finding the T cells will be accepted by recipients with only one matching HLA allele - which makes a T cell bank feasible.
“If you think of all the different tissue types in the community and you only need to be matched at one, you can cover just about everybody, because even if they are not matched to the rare HLA alleles most people will have a certain number of the common ones,” said Blyth.
Trialling off the shelf
A trial the team is currently running is looking at transitioning to use these off-the-shelf T cells. This multisite study opened in Australia and New Zealand at the end of 2012 and the researchers have been working on optimising manufacturing protocols for it.
In the first part of this work they identified target donors of common HLA types then took their optimised manufacturing protocols and grew up individual products with CMV, EBV or adenovirus specificity to large numbers in the lab. They then aliquoted them into smaller amounts and froze them individually.
“We then test each of those individual units to make sure they recognise the virus of interest,” said Clancy. “Importantly, we also test them to determine which HLA type that antiviral activity is being directed through. If we know that information and we have a patient with a problem, if we know that patient’s particular tissue type then we can go to the bank and select the most appropriate product for them. In this way, T cells can be provided to patients in need within 1-2 days whereas the process of growing cells specifically for a patient on demand takes 5-6 weeks.”
This trial is ongoing. The researchers cite logistical barriers as preventing things from progressing too quickly.
“Having the infrastructure to create a bank and the resources to maintain it is a big challenge,” said Blyth. “These sorts of practicalities are limiting and we are only a small outfit.
“One of the important things is to demonstrate that it’s cost effective and we are still working towards this,” she continued. “If we can prove to the CEO that his bottom line will be better then there’s impetus to fund the infrastructure.”
Then there are the regulatory hurdles to get through.
Meeting Therapeutic Goods Administration (TGA) standards can be a huge task and applying for TGA licensure for products for use in humans - in this case a different product for each patient - can cost millions. Add to this setting up the infrastructure and having quality systems in place and the hurdles get pretty big for an investigator-driven project.
T cells to treat cancer
Yet another area the researchers are looking into is treating the cancer itself by with T cells.
This would address a big area of need - developing a treatment for transplant patients who relapse and die from their original disease.
“We could do this in two ways,” said Blyth. “First, we could get T cells specific for tumour antigens from donors - we’ve been looking into this for a while and it’s in preclinical phase at the moment; the other way is to modify the T cells genetically to make them specific to the tumour so they attack it.”
Haematologist Dr Ken Micklethwaite is working with them to look at genetically modifying T cells that specifically target B cell tumours.
In this technique, the T cells are modified or reprogrammed to carry the gene for a chimeric antigen receptor - a modified T cell receptor that is specific for the antigen in question.
“We use a non-retrovirus system, a transposon-transposase plasmid-based system to deliver the genes,” explained Clancy, “that avoids the need for using retrovial systems and the hurdles associated with that.”
In their case, the T cells are being modified to confer specificity to CD19, an antigen on B cells. The T cells then specifically target B cell tumours.
Although it’s early days, this work is producing exciting results.
“People with end-stage completely treatment resistant disease get spectacular complete cures because the T cells go in, proliferate against the antigen target and kill the tumour,” Blyth said, citing other studies that have been conducted in this area.
The long-term vision is to combine the viral-specific T cells with the tumour-specific T cells to develop a post-transplant treatment package for patients.
“If this approach was effective, theoretically it could decrease post-transplant deaths by 70%,” said Blyth.
“The ultimate goal would be that it’s clinically incorporated into routine practice. Patients would come in and get their stem cell transplant, they get their complete antiviral, antitumour T cells grown from the stem cells at the same time and have a much better time of it.”
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...
Clogged 'drains' in the brain an early sign of Alzheimer’s
'Drains' in the brain, responsible for clearing toxic waste in the organ, tend to get...
World's oldest known RNA extracted from woolly mammoth
The RNA sequences are understood to be the oldest ever recovered, coming from mammoth tissue...



