Bird flu update: raw milk risk, experimental vaccine developed
Australia was rocked by several cases of avian influenza (bird flu) last week — with two Victorian egg farms infected by the H7N3 subtype of the virus, the low pathogenic H9N2 detected in a Western Australian mixed poultry farm and one human case of H5N1 in a returned traveller. With the affected farms quarantined and hundreds and thousands of birds euthanased, health departments have made it clear that poultry products remain safe to consume, so long as they are thoroughly cooked before eating (with hands washed after handling raw ingredients). But what about dairy products?
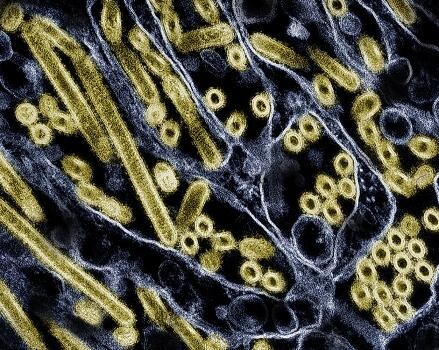
Avian influenza primarily affects wild birds and poultry, with a rare number of human cases primarily among people who have had close contact with infected birds. In the past few years, however, a strain of highly pathogenic avian influenza (HPAI) H5N1 has spread to infect more than 50 animal species, and in late March, the United States reported a viral outbreak among dairy cows in Texas. To date, 52 cattle herds across nine states have been affected, with two human infections detected in farm workers with conjunctivitis.
To assess the risk of H5N1 infection by consuming raw milk, researchers from the University of Wisconsin–Madison and Texas A&M Veterinary Medical Diagnostic Laboratory fed droplets of raw milk from infected dairy cattle to five mice. The animals demonstrated signs of illness, including lethargy, on day one and were euthanased on day four to determine organ virus levels. The researchers discovered high levels of virus in the animals’ nasal passages, trachea and lungs and moderate-to-low virus levels in other organs, consistent with H5N1 infections found in other mammals. Their results were published in The New England Journal of Medicine.
In addition to the mice studies, the researchers also sought to determine which temperatures and time intervals inactivate H5N1 virus in raw milk. Four milk samples with high H5N1 levels were tested at 63°C for 5, 10, 20 and 30 min, or at 72°C for 5, 10, 15, 20 and/or 30 seconds. Each of the time intervals at 63°C successfully killed the virus. At 72°C, virus levels were diminished but not completely inactivated after 15 and 20 seconds (the authors emphasise, however, that their laboratory study was not identical to large-scale industrial pasteurisation of raw milk). In a separate experiment, the researchers stored raw milk infected with H5N1 at 4°C for five weeks and found only a small decline in virus levels, suggesting that the virus in raw milk may remain infectious when maintained at refrigerated temperatures.
According to the US Food and Drug Administration (FDA), the totality of evidence continues to indicate that the commercial milk supply is safe. However, the research results underscore the opportunity to conduct additional studies that closely replicate real-world conditions. The FDA, in partnership with US Department of Agriculture, is now conducting pasteurisation validation studies, including the use of a homogeniser and continuous flow pasteuriser.
mRNA vaccine breakthrough
Meanwhile, researchers at the University of Pennsylvania have developed an experimental mRNA vaccine against H5N1 that is highly effective in preventing severe illness and death in preclinical models. Described in the journal Nature Communications, the vaccine could help manage the outbreak of the H5N1 virus before it has the chance to evolve and cause a human pandemic.
Most influenza vaccines are egg-based, where experts inject fertilised chicken eggs with what they predict will be the dominant viral strain, let it replicate and then inactivate the virus to use in the flu shots distributed globally. However, viruses must first be adapted to replicate in fertilised eggs before these conventional vaccines can be produced, which can take up to six months, presenting potential problems for quickly producing vaccine when it’s needed most during the first few months of a pandemic. mRNA vaccines are easily and quickly adapted to protect against different strains of influenza viruses, and don’t require eggs for their development.
“mRNA technology allows us to be much more agile in developing vaccines; we can start creating an mRNA vaccine within hours of sequencing a new viral strain with pandemic potential,” Professor Scott Hensley said. “During previous influenza pandemics, like the 2009 H1N1 pandemic, vaccines were difficult to manufacture and did not become available until after the initial pandemic waves subsided.”
Hensley and his team collaborated with the laboratory of mRNA vaccine pioneer and Nobel Prize winner Professor Drew Weissman, Director of Vaccine Research at Penn Medicine. Together, they developed an mRNA vaccine targeting a specific subtype of the H5N1 virus that is circulating widely in birds and cattle.
The researchers found that the vaccine elicited a strong antibody and T cell response in mice and ferrets, with the animals maintaining high levels of antibodies even a year after vaccination. Additionally, vaccinated animals who were subsequently infected with H5N1 cleared the virus more rapidly and displayed fewer symptoms than unvaccinated controls. The researchers also noted that all of the vaccinated animals survived following H5N1 infection, whereas all the unvaccinated animals died.
Finally, the team compared the mRNA vaccine response in mice to their response to a traditional egg-based vaccine and found that the mRNA vaccine was just as effective. Both vaccines elicited strong antibody responses, regardless of prior seasonal flu exposures.
“Before 2020, experts thought the influenza virus posed the greatest risk of causing a pandemic, and we had limited options for creating a vaccine if that had happened,” Weissman said. “COVID-19 showed us the power of mRNA-based vaccines as a tool to protect humans from emerging viruses quickly, and we are better prepared now to respond to a variety of viruses with pandemic potential, including influenza.”
Single-cell sequencing capability boosted in South Australia
The South Australian Genomics Centre has become the first certified service provider in...
Biomaterial helps to reverse aging in the heart
The discovery could open the door to therapies that rejuvenate the heart by changing its cellular...
mRNA used to force HIV out of hiding
Using the same technology behind mRNA COVID-19 vaccines, researchers have discovered a way to...








