How cancer grows resistant to treatment
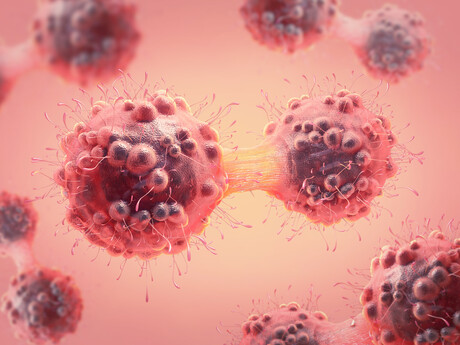
The cells of the human body are constantly dividing, and each time they need to copy a three billion-letter DNA code with high precision to ensure cell survival. It turns out that the same is not true for cancers, a broad range of which — including melanoma, pancreatic cancer, sarcomas and breast cancer — generate a high number of errors when they copy their DNA when exposed to cancer treatments, leading to drug resistance.
These are the findings of an Australian research team, led by Professor David Thomas at the Garvan Institute of Medical Research. Writing in the journal Science, the team revealed that cancer cells can ‘turn on’ error-prone DNA copy pathways to adapt to cancer treatment — the same process used by bacteria to develop antibiotic resistance.
Researchers have long known that cancer cells accumulate genetic variations that make it possible for them to evade treatment. But how this happens — and whether the process could be targeted to improve cancer treatment — has been elusive.
The Australian scientists began to investigate the underlying drivers of treatment resistance by analysing biopsy samples from cancer patients, before and after they were treated with targeted cancer therapies. Targeted therapies block the growth of cancer by interfering with molecules that are needed for tumour growth, and are a common treatment for many forms of cancer.
The scientists were surprised to discover that the cancer cells from patients that had received targeted therapies showed much higher levels of DNA damage than pre-treatment samples — even when these treatments did not directly damage DNA. Further, the researchers used whole-genome sequencing to analyse how treatment resulted in accelerated evolution of the cancer genome.
“Our experiments revealed that cancer cells exposed to targeted therapies undergo a process called stress-induced mutagenesis — they generate random genetic variation at a much higher rate than cancer cells not exposed to anticancer drugs,” said first author Dr Arcadi Cipponi, from the Garvan Institute and UNSW.
“This process is ancient — single-celled organisms, such as bacteria, use the same process to evolve when they encounter stress in their environment.”
To pinpoint the mechanisms underlying stress-induced mutagenesis in human cancer cells, the researchers carried out a large-scale screen to silence every gene in cancer cells individually, looking to identify the specific pathways contributing to drug resistance. When they silenced the gene for MTOR — a stress sensor protein — they discovered that cancer cells stopped growing, but paradoxically accelerated evolution in the presence of a cancer treatment.
“MTOR is a sensor protein that tells normal cells to stop growing because there is a stress in the environment,” Dr Cipponi said. “But we found that in the presence of a cancer treatment, MTOR signalling allowed cancer cells to change expression of genes involved in DNA repair and replication, for example shifting from high-fidelity polymerases, the enzymes that copy DNA, to production of error-prone polymerases. This resulted in more genetic variation, ultimately fuelling resistance to treatment.”
The shift to low-fidelity DNA repair and replication was temporary — once cancer cells acquired resistance to a cancer treatment, they reactivated high-fidelity pathways.
“Genomic instability can itself be harmful to cells, which is why some of our chemotherapies and therapeutic radiation work,” Dr Cipponi said. “We found that once cancer cells had developed resistance to a treatment, they switched back to high-fidelity DNA polymerases to ensure the cells that had evolved resistance to treatment could survive.”
Combining conventional targeted cancer therapy with drugs that target DNA repair mechanisms may lead to more effective therapeutic strategies, the researchers claim. As a proof of principle, they tested such a drug combination in a mouse model of pancreatic cancer. By combining the cancer treatment palbociclib with rucaparib, a drug which selectively targets cells with impaired DNA repair, they were able to reduce cancer growth by almost 60% over 30 days compared to palbociclib alone.
“Resistance to treatment is arguably the major issue facing patients with advanced cancers, for whom even effective treatments ultimately fail,” said Prof Thomas, Garvan’s Cancer Research Theme Leader and Director of The Kinghorn Cancer Centre.
“Our findings have opened up new potential strategies that either prevent stress-induced mutagenesis in cancers or are more effective in cancers that have already developed resistance.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...
Clogged 'drains' in the brain an early sign of Alzheimer’s
'Drains' in the brain, responsible for clearing toxic waste in the organ, tend to get...
World's oldest known RNA extracted from woolly mammoth
The RNA sequences are understood to be the oldest ever recovered, coming from mammoth tissue...





