Light-activated drugs for pain treatment
Scientists from Spain, France and Italy have designed what is claimed to be the first light-activated drug for the treatment of pain, making a major step for the discipline of optopharmacology (the use of light to control drug activity). Their research has been published in the journal eLife.
The advantage of using light on a photosensitive drug, explained the researchers, is that the pharmacological process can be controlled with spatial and temporal precision. Now, the team have designed a ‘photo-drug’, called JF-NP-26, with powerful therapeutic applications to treat pain — an area which has so far been underexplored in optopharmacology. The key lies in a molecule that can be activated at any moment with light.
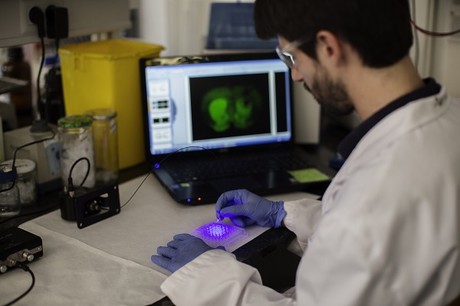
The researchers proposed that a drug with a known action mechanism (eg, an analgesic) be chemically modified to make it photosensitive and inactive. The drug would then be activated when receiving light — using an optical fibre — of a suitable wavelength and with exact precision on the target tissue (brain, skin, articulations, etc). The design was tested on the photocaged drug JF-NP-26 — a chemically and inactive covered molecule which was subsequently activated with light.
The drug’s lightening includes a treatment on the molecule that releases the active molecule (raseglurant) that blocks the metabotropic glutamate type 5 (mGlu5) receptor, found in neuronal functions such as the spread of neuronal pain. Blocking this receptor prevents the pain from spreading into the brain. This can be produced both due to the outlying neurons and the central nervous system (brain) and create, in both cases, an analgesic effect as a result.
“The molecule created by the action of the light, the raseglurant, does not belong to any group of drugs from the classic anti-pain list of drugs: non-steroidal anti-inflammatory drugs or NSAID (paracetamol, ibuprofen, etc) and opioids (morphine, phentanyl),” said Professor Francisco Ciruela from the University of Barcelona.
“The raseglurant was examined in clinical trials as an analgesic to treat migraine, but it was ruled out due its hepatoxicity. This new optopharmacology of the raseglurant can stop adverse effects in the liver and opens a new path to start using it as an analgesic.”
Compared to other photosensitive compounds, the molecule was found to have no pharmacological effect on an animal until the target tissue received light from a visible spectrum (405 nm wavelength). Moreover, JF-NP-26 did not show toxic or unwanted effects, even in high doses, in short-length studies on animals.
The scientists believe the discipline of optopharmacology will help widen the therapeutic range to treat pain and notably reduce the unwanted effects several drugs (eg, the high risk of addiction in morphine, the NSAID low analgesic efficacy in severe and chronic pain, etc). They are now working on research lines in optopharmacology to respond to problems related to conventional pharmacology.
“At this moment we are examining other molecules with different action mechanisms but also based on G protein-coupled membrane receptors, the biggest therapeutic target at the moment,” said Ciruela. “Therefore, we have drugs under study for the treatment of Parkinson’s disease or psoriasis. We are also exploring the optopharmacological use of light with different wavelengths (green, yellow and red) which are even less toxic.
“Regarding the future, we cannot rule out some symptomatology to be lowered with optical fibres in the brain, just like electrodes are put in the deep brain stimulation with Parkinson’s disease.”
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...
Clogged 'drains' in the brain an early sign of Alzheimer’s
'Drains' in the brain, responsible for clearing toxic waste in the organ, tend to get...
World's oldest known RNA extracted from woolly mammoth
The RNA sequences are understood to be the oldest ever recovered, coming from mammoth tissue...



