New ways to beat chronic pain
Pain is expected to subside as injuries heal, but many patients experience persistent pain long after recovery. Now, a new study published in Science Translational Medicine points to possible treatments for chronic pain with a surprising link to lung cancer.
The work was spearheaded by an international team of researchers at the Institute of Molecular Biotechnology of the Austrian Academy of Sciences (IMBA), Harvard Medical School and Boston Children’s Hospital. Their findings from the research, conducted in laboratory mouse models, open up multiple therapeutic opportunities that could allow the world to improve chronic pain management and eclipse the opioid epidemic.
Acute pain is an important danger signal. By contrast, chronic pain is based on persistent injury and can even be experienced in the absence of a stimulus, injury or disease. To improve how persistent pain is managed and considering the raging opioid crisis, it is paramount to develop novel drugs based on a fundamental understanding of the underlying mechanisms.
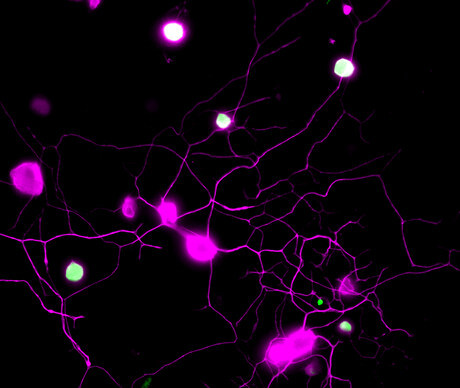
“We had previously shown that sensory neurons produce a specific metabolite, BH4, which then drives chronic pain, such as neuropathic pain or inflammatory pain,” said project lead and co-corresponding author Shane Cronin, a staff scientist at IMBA and former postdoc at Harvard Medical School and Boston Children’s Hospital. “The concentrations of BH4 correlated very well with the pain intensity. So we naturally thought that this was a great pathway to target.”
To identify drugs that reduce BH4 levels in pain neurons, the researchers performed a ‘phenotypic screen’ of 1000 target-annotated, FDA-approved medications. This approach allowed the scientists to start their search using medications that are currently in use for various indications, and to identify undescribed, off-target analgesic properties. Among the first findings of this hypothesis-driven search, the team was able to link the previously observed analgesic effects of several drugs, including clonidine and capsaicin, to the BH4 pathway.
“However, our phenotypic screen also allowed us to ‘repurpose’ a surprising drug,” Cronin said, referring to an antipsychotic known as fluphenazine which is used to treat schizophrenia.
“We found that fluphenazine blocks the BH4 pathway in injured nerves; we also demonstrated its effects in chronic pain following nerve injury in vivo,” Cronin said. The researchers also found that the effective analgesic dose of fluphenazine in their experiments in the mouse model is comparable to the low end of the doses safely indicated for schizophrenia in humans.
In addition, the screen uncovered a novel and unexpected molecular link between the BH4 pathway and EGFR/KRAS signalling, a pathway involved in multiple cancers. Blocking EGFR/KRAS signalling reduced pain sensitivity by decreasing the levels of BH4. The genes of EGFR and KRAS are the two most frequently mutated genes in lung cancer, which prompted the researchers to look at BH4 in lung cancer.
Surprisingly, by deleting an important enzyme, GCH1, in the BH4 pathway, the mouse models of KRAS-driven lung cancer developed fewer tumours and survived much longer. Hence, the researchers uncovered a common signalling pathway for chronic pain and lung cancer through EGFR/KRAS and BH4, thus opening up new avenues of treatment for both conditions.
One intriguing aspect of the study is the mechanistic link between pain and lung cancer. As noted by co-corresponding author Josef Penninger, IMBA group leader and founding director, “The same triggers that drive tumour growth appear to be also involved in setting the path to chronic pain, often experienced by cancer patients. We also know that sensory nerves can drive cancer, which could explain the vicious circuit of cancer and pain. Understanding these cross-talks is therefore not only critical for cancer treatments but might also help to improve the quality of life for cancer patients towards less pain.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
How cells repair toxic DNA damage
Researchers say they have uncovered the mechanism by which cells identify and repair a highly...
Sequencing tech could transform NZ viticulture
A new initiative aims to utilise genomics to breed better varieties of grapevines and hops that...
Eight babies born in UK following mitochondrial donation
The birth of eight babies with a greatly reduced risk of developing mitochondrial DNA disease...




