Retuning tired T-cells
A team of researchers from the University of New South Wales have been zooming in on individual molecules to determine how our immune system’s T-cells respond to threats — and what they’ve found could revolutionise the way we treat certain diseases.
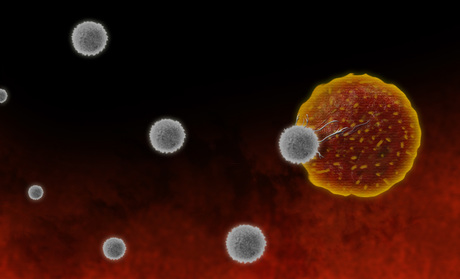
For our immune system to be effective, T-cells need to recognise potentially dangerous antigens and warn the nucleus that it is time to attack. They do this with tiny receptors that bind to the antigens, translating biochemical activity outside the cell into warning signals.
“But these receptors do more than just flick a switch to tell the cell ‘yes’ or ‘no’,” said UNSW Scientia Professor Katharina Gaus. “It’s almost like they have an artificial intelligence. They translate the complex biochemical binding event outside the cell into a warning signal, and they encode the level of response that’s needed to effectively counteract the threat at the exact right time.”
One unexpected observation is that only a quarter of a T-cell’s receptors activate when exposed to antigens and this performance disparity appears to be linked to spatial organisation on the cell’s surface. Lead author Dr Sophie Pageon explained: “If they’re clustered together in a crowded environment, they’re much more likely to switch on than a receptor with no neighbours around it.”
This could lead to far more effective treatments for cancer and other diseases, according to Professor Gaus. “Without reprogramming or genetically changing the whole T-cell, we can tune its sensitivity by corralling the receptors together, so they are densely clustered on the surface of the cell in a more optimal distribution.
“In people with cancer, for example, T-cells eventually become inactive or exhausted. Taking what we now know about the T-cell clusters, we can develop strategies to rescue these T-cells, and turn the receptors back on.”
A nanotechnology device for rearranging T-cell receptors is already in development and experiments in mouse models are simply awaiting funding.
This is the first time that powerful imaging technology, including Australia’s only super-resolution microscopes, has been used to zoom in and view this critical first stage in the immune response. Professor Gaus said the UNSW Single Molecule Science lab enabled the researchers to “pinpoint this process by imaging individual molecules in single T-cells, and going right down to the molecular level to see how this mechanism works”.
The research was funded by the Australian Research Council and the National Health and Medical Research Council of Australia, under the auspices of the ARC Centre of Excellence in Advanced Molecular Imaging. It was published in the Proceedings of the National Academy of Sciences.
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...
Clogged 'drains' in the brain an early sign of Alzheimer’s
'Drains' in the brain, responsible for clearing toxic waste in the organ, tend to get...
World's oldest known RNA extracted from woolly mammoth
The RNA sequences are understood to be the oldest ever recovered, coming from mammoth tissue...



