Specially designed peptides can treat complex diseases
Two separate research teams have found ways to create short chains of amino acids, termed peptides, for the purpose of treating a variety of diseases — including cancer.
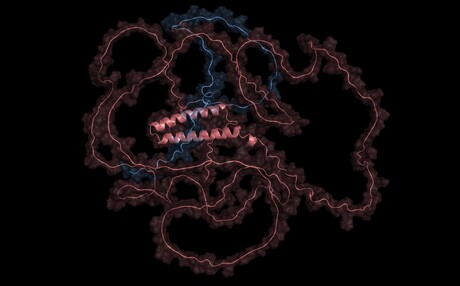
One approach to treat disease is to develop therapeutics that can specifically target and destroy the proteins driving it. Sometimes these key proteins have well-defined structures, like a neatly folded origami crane, so conventional small molecule therapies can easily bind to them. But more than 80% of disease-causing proteins instead resemble a messy ball of yarn — disordered and tangled — making it difficult for standard therapies to find a pocket on the surface to latch on and do their job.
To circumvent this issue, researchers have explored how peptides can be used to bind to and degrade disease-causing proteins. Because peptides are small versions of proteins, they don’t require surface pockets for binding. Instead, they can bind to various amino acid sequences throughout the protein. But even these approaches have their limits, as existing ‘off-the-shelf’ binders have not been designed to attach to unstable or overly tangled protein structures. While scientists have been working on developing new binding proteins, these approaches still rely on mapping out the 3D structural information of the target protein, which is not available for disordered targets.
Rather than try to map out the structures of disease-causing proteins, Assistant Professor Pranam Chatterjee and his team of biomedical engineers at Duke University took inspiration from generative large language models (LLMs) to create a solution. The result, described in the journal Science Advances, is PepPrCLIP, or Peptide Prioritization via CLIP.
The first component of the tool, PepPr, uses a generative algorithm trained on a vast library of natural protein sequences to design new ‘guide’ proteins with specified characteristics. CLIP, the second component of the platform, utilises an algorithm framework, initially developed by OpenAI to match images and corresponding captions together, to test and screen which of these peptides match with their targeted proteins. The CLIP model here only requires the target sequence.
“OpenAI’s CLIP algorithm connects language with an image,” Chatterjee explained. “If you have text that says ‘dog’, you should get an image of a dog. Instead of language and image, we trained it to match peptides and proteins. PepPr makes the peptides, and our adapted CLIP algorithm will screen those peptides and tell us which ones will make a good match.”
In a comparison against RFDiffusion, an existing platform for generating peptides using the 3D structure of a target, PepPrCLIP was faster and was able to create peptides that were almost always a better match for their targeted protein. To gauge how well PepPrCLIP could work with both ordered and disordered protein targets, Chatterjee and his lab teamed up with researchers from Duke University Medical School, Cornell University and Sanford Burnham Prebys Medical Discovery Institute to experimentally test the platform.
In the first test, the team showed that PepPrCLIP-generated peptides could effectively bind to and inhibit the activity of UltraID, a relatively simple and stable enzyme protein. Next, they used PepPrCLIP to design peptides that could attach to beta-catenin — a disordered, complex protein involved in signalling for several different types of cancer. The team generated six peptides that CLIP indicated could bind to the protein and showed that four could effectively bond to and degrade their target. By destroying the protein, they can slow down cancer cell signalling.
In their most complicated test, the team designed peptides that could bind to a highly disordered protein affiliated with synovial sarcoma — a rare, aggressive cancer that can develop in soft tissue and mostly affects children and young adults. According to Chatterjee, “It’s like a bowl of spaghetti; it’s the most disordered protein in the world.”
The team tested 10 designs by putting their peptides into synovial sarcoma cells. They observed that the PepPrCLIP-designed peptides could both bind and degrade the protein, just as it had with simpler targets. And if they can destroy the protein, they have an opportunity to develop a therapy for a previously undruggable cancer.
Beyond plans to continue to improve their platform, Chatterjee and his team plan to partner with medical and industry professionals to begin creating peptides that could eventually be used in new therapies for diseases caused by unstable proteins like Alexander disease, a fatal neurological disease that primarily affects children, and different types of cancers. According to Chatterjee, “These complex, disordered proteins have made a lot of cancers and diseases practically undruggable because we couldn’t design molecules that bind to them” — but PepPrCLIP has shown that it can work on even the most complicated protein, which opens up a lot of exciting clinical possibilities.
Enhancing efficacy
In a separate study, published in the journal Chem, scientists from the City University of New York (CUNY) and Memorial Sloan Kettering Cancer Center revealed how they are using specially designed peptides to improve drug formulations. This innovative method was found to significantly enhance anti-tumour efficacy, as demonstrated in leukaemia models.
The researchers set out to solve two critical challenges faced by drug delivery systems: poor solubility and inefficient delivery within the body. Many drugs do not dissolve well, making it difficult for them to reach their intended targets. Furthermore, current delivery systems waste a significant portion of the drug during preparation — only 5–10% of the drug is successfully loaded, leading to less effective treatments.
The research team has developed a novel solution by designing peptides to bind with specific drugs and create therapeutic nanoparticles. These nanoparticles are primarily composed of the drug, with a thin peptide coating that improves solubility, enhances stability in the body and optimises delivery to targeted areas. This approach was found to achieve drug loadings of up to 98%, a dramatic improvement over traditional methods.
By using a combination of computer models and laboratory tests, new drug/peptide nanoparticles were identified. These subsequently demonstrated remarkable results in leukaemia models, with the nanoparticles proving more effective at shrinking tumours compared to the drugs alone. Additionally, their high efficiency allows for lower doses of drugs, potentially reducing the side effects.
“Peptides, which are designed molecules made from the same building blocks as the proteins in our body, are extremely versatile,” said co-principal investigator Rein Ulijn, Director of the Nanoscience Initiative at CUNY’s Advanced Science Research Center and a chemistry professor at Hunter College. “We thought they could be useful in solving two big problems seen in many drugs: poor solubility and inefficient delivery. By designing a peptide that binds the drug while enhancing its solubility, we were able to create nanoparticles with very high loading.”

The researchers believe their innovation holds significant potential because peptides can be customised to enhance the effectiveness of various drugs. Given the vast range of possible interactions in peptide design, they say it may be feasible to tailor peptides for specific drugs, extending their applicability beyond cancer treatments.
“This breakthrough enables the development of better precision medicines,” said co-principal investigator Daniel Heller, Head of the Cancer Nanomedicine Laboratory at Memorial Sloan Kettering Cancer Center’s Molecular Pharmacology Program. “Using specially designed peptides, we can build nanomedicines that make existing drugs more effective and less toxic and even enable the development of drugs that might not be able to work without these nanoparticles.”
The research team is now adopting lab automation methods to further refine and accelerate the peptide-drug matching process. Their next steps include verifying the approach’s potential in a wider range of diseases. If successful, this innovation could lead to more effective treatments, reduced side effects, and significant cost savings in drug development.
“It’s incredible to see how simple variations in peptide sequence could match specific drugs,” said Naxhije ‘Gia’ Berisha, a former CUNY Graduate Center PhD student who performed much of the experimental work. “This suggests there may be a peptide match for every drug, potentially revolutionising the way medicines are delivered.”
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...
Clogged 'drains' in the brain an early sign of Alzheimer’s
'Drains' in the brain, responsible for clearing toxic waste in the organ, tend to get...
World's oldest known RNA extracted from woolly mammoth
The RNA sequences are understood to be the oldest ever recovered, coming from mammoth tissue...



