Targeted therapy for childhood brain cancer shows promise
A research team led by QIMR Berghofer and Emory University has shown that a potential new targeted therapy for childhood brain cancer is effective in infiltrating and killing tumour cells in preclinical models. The researchers said their findings, which have been published in the journal Nature Communications, are potentially transformative for the treatment of the most common childhood brain cancer (medulloblastoma) and could apply to other brain cancers as well.
Brain cancer is the second leading cause of death in children in the developed world. For the children who survive, standard treatments have long-term impacts on their development and quality of life, particularly in small children and infants. When medulloblastoma recurs, the prognosis is usually extremely poor.
“Current treatments, including radiation and chemotherapy, often eliminate most of the tumour, but sometimes fail to eliminate cancer stem cells,” said Emory University Professor Timothy Gershon. “These cancer stem cells can regrow the tumour after treatment, causing fatal recurrence.”
The research teams collaborated with US biopharmaceutical company Curtana Pharmaceuticals, which has developed an experimental drug called CT-179. The researchers found that the drug effectively targets the protein OLIG2, which is a known stem cell marker crucial in the initiation and recurrence of brain cancers.
“We show that CT-179 treatment specifically disrupts cancer stem cells,” said Gershon, who is also a paediatric neurologist at Children’s Healthcare of Atlanta and Director of the Children’s Center for Neurosciences Research.
“Combining CT-179 with treatments such as radiation therapy treats the whole tumour more effectively, including both stem cells and tumour cells that are not stem cells. Adding CT-179 to combinations of treatments may bring new efficacy to brain tumour therapy.”
Professor Bryan Day, who leads QIMR Berghofer’s Sid Faithfull Brain Cancer Laboratory and is Co-Director of the Children’s Brain Cancer Centre, described the findings as a breakthrough, made more significant because they result from independent studies.
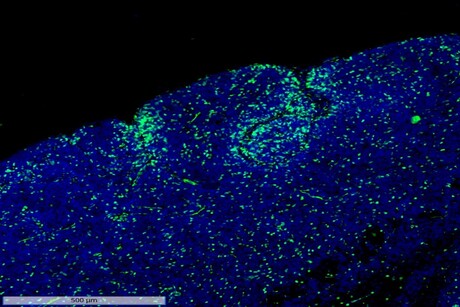
“Children with brain cancer urgently need more effective and less toxic treatments,” Day said. “Our study demonstrated that the drug CT-179, used in combination with standard radiation therapy, can cross the blood–brain barrier and penetrate the tumour. It prolonged survival in a range of preclinical medulloblastoma models, delayed recurrence of the disease, and increased the effectiveness of radiotherapy.”
QIMR Berghofer postdoctoral researcher Dr Yuchen (Michelle) Li, who was joint first author on the study, noted that the blood–brain barrier is a big obstacle in terms of treating brain cancer.
“As a small molecule drug, CT-179 can penetrate the blood–brain barrier and could also be taken orally, making it easier to administer to young patients,” Li said.
“In our experimental models in the lab, the drug ‘hangs around’ in the brain. When used in combination with radiotherapy, the hope is that overall treatment is more effective and less toxic, which reduces the long-term therapy-induced side effects that have such an impact on patients.”
The team’s findings complement the results of another study, published concurrently in Nature Communications, led by Professor Peter Dirks from the University of Toronto. That study identified the OLIG2 protein as a key regulator of the tumour’s growth transitions and presented a novel therapeutic angle, highlighting a shift from general tumour treatment to precise interventions targeting tumour-initiating cells.
“Our study demonstrated that the OLIG2 protein is a critical driver of the complex early stages of medulloblastoma tumor formation, making it a highly promising treatment target,” said Dirks, who is also Neurosurgeon-In-Chief and a Senior Scientist at The Hospital for Sick Children.
“We showed that inhibiting the OLIG2 protein with the CT-179 drug prevented cancer stem cells from changing to a proliferative state, effectively blocking the growth and recurrence of tumours. This could have potentially profound implications for treatment in the future.”
With both studies now published, Day said the next step is to undertake clinical trials.
“We’ve been working hard toward this goal with our collaborators, particularly in the United States and here in Australia, and we are now seeking funding to advance to first-in-human clinical testing of CT-179 in patients with brain cancer,” he concluded.
Breakthrough drug prevents long COVID symptoms in mice
Mice treated with the antiviral compound were protected from long-term brain and lung dysfunction...
Antibiotics hinder vaccine response in infants
Infants who received antibiotics in the first few weeks of life had significantly lower levels of...
Colossal announces 'de-extinction' of the dire wolf
Colossal Biosciences has announced what it describes as the rebirth of the dire wolf, which would...




