Transgenic livestock, by half measures
Tuesday, 06 December, 2005
Manipulating the genome before fertilisation could prove more successful that current technique used in animal transgenesis, Graeme O'Neill reports.
Sperm-mediated transgenesis -- a modern wrinkle on nature's time-honoured mode of reproduction, is potentially a more efficient way to create 'designer' livestock animals, US animal geneticist Dr Ina Dobrinski told the recent CSIRO Horizons in Livestock Science conference.
Dobrinski, from the Centre for Animal Transgenesis and Germ Cell Research at the University of Pennsylvania, said techniques like pronuclear microinjection and somatic cell nuclear transfer (SCNT) are expensive, time-consuming and typically very inefficient.
Historically, Dobrinski said, livestock breeds were improved by humans selecting superior phenotypes; modern breeding is increasingly based on genetic analysis, and gene targeting.
Developing transgenic animals exhibiting improved production traits and disease resistance was the most obvious, but most difficult way to proceed -- transgenic animals could also be used in research, or as a source of 'humanised' organs for transplant surgery.
Pronuclear microinjection and SCNT both involve manipulating oocytes, or early-term embryos; with both, epigenetic errors -- gene imprinting -- can cause developmental problems. Manipulating the genome before fertilisation could avoid these problems, Dobrynski said.
From rats to pigs to primates
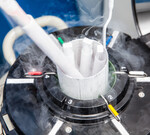
The technique involves germ-cell transplantation to create transgenic animals by manipulating spermatogonia -- a self-renewing population of male germ-line stem cells residing in the basement membrane of the testis that undergo mitotic division to produce sperm.
All male germline cells are destined to die within the individual, but possess the potential to transmit genes to the next generation. "They're difficult cells to work with," Dobrinski said. "Not the least problem is that we still don't know for sure which ones are stem cells."
In 1994 University of Pennsylvania researcher Dr Ralph Finster made a cell suspension from the testis of a donor animal, transplanted it into a sterile male of the same species, and showed that the donor germline cells colonised and functioned normally in the infertile animal's testis.
When mated to wild-type females, the formerly infertile males sired a number of normal progeny. Finster was able to track the donor cells by inserting a Lac operon -- in the process, he created a functional reconstitution assay for male germline stem cells.
"About 99 per cent of research on germ cell transplantation today involves rodents," Dobrinski said. "All the reagents and tools are in place. But we're trying to engineer livestock species like cattle, pigs, goats and non-human primates -- we were fascinated by the idea that we could apply our experience with the rodent system to study a much larger species like the pig.
"We had shown we could transfer rat germline cells into mouse testes and get them to produce sperm, and it also worked in a hamster-to-mouse experiment."
Immunologically privileged
The University of Pennsylvania researchers found they could grow colonies of pig germ cells in mouse testes; in mammals, the testes are an immunologically privileged tissue, protected against attack by antibody-secreting B cells and cytotoxic T cells.
Since then, they have shown they can also grow rabbit, dog, bull, horse and primate cells in mouse testes -- but the cells do not enter into meiosis and create sperm.
"The first step for the germ cell is to recognise it is in the mouse, but something is missing in the new environment -- we can't get mature gametes to form," Dobrinski said.
If this problem can be solved, the attraction of the technique -- called xenogeneic spermatogonial transplantation -- is that researchers only have to deal with a small, easily manipulated animal, to make transgenic gametes form other, much larger species.
As an example of the potential utility of the technique, Dobrinski said her team had transplanted germline cells from a transgenic male goat carrying a human alpha-antitrypsin gene, under the control udder-specific promoter, into the testis wild-type goats.
They subsequently detected the sperm-derived transgene in the ejaculates of two out of five of the treated goats, and when one of the males was mated to a wild-type female, one of the 15 offspring was transgenic for the donor-derived transgene.
"So we have provided proof of principle that it is possible to take germ cells from a donor animal, transplant them into a pure-bred animal, and then mate it to a wild-type female, and some of the progeny will carry the donor transgene.
"All our rodents were either syngeneic, or immunosuppressed, but the goats were unrelated and immunologically competent -- it works between unrelated individuals of livestock species, which is a huge advantage.
"And the technology is easily transferable to other species -- the University of California, Davis, has demonstrated it in a rhesus monkey model, and Dr John Hill at CSIRO Armidale has done it in a bovine model."
The germ cell niche
The challenge is in the preparation of the recipient animals. "We want the recipient animal to make a majority of sperm with the genotype of the donor animal," Dobrinski said. "We can decrease or eliminate the germ cells of the recipient using post-natal treatment with busulfan, a cytotoxic cancer drug, or testicular irradiation.
"But the donor germ cells are more likely to stay in residence and replicate if the testis is healthy, so we're not aiming at complete elimination of the recipient's germ cells."
Other problems to be solved include isolating and enriching donor germ cells to produce a homogeneous population, then to achieve efficient stable integration of transgenes into testis cells -- no easy matter. Germ cells are niche specialists, with very specific requirements; they also replicate slowly, making them inherently 'finicky' to culture.
Dobrinski's team has experimented with lipofection, electroporation, a gene 'gun', various adenovirus, retrovirus and lentivirus vectors. Adeno-associated virus provided the first success in 2000.
The technique would save a lot of time, Dobrinski said. "You transfect the cells, transplant them into males, wait for them to produce sperm, then collect it."
How a common gene mutation increases liver disease risk
Liver damage can be caused in people after exposure to high levels of acrolein, especially in...
Gene therapy slows Huntington's disease progression in trial
Patients receiving the treatment were found to experience 75% less progression of the disease...
AI-driven manufacturing: lessons from the life sciences industry
The use of artificial intelligence for batch monitoring and digital twin development is...