A pre-emptive approach to treating leukaemia relapse
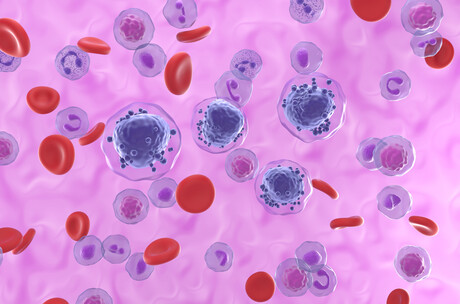
A research team led by the Peter MacCallum Cancer Centre (Peter Mac) has revealed how the monitoring of measurable residual disease (MRD), medication and low-dose chemotherapy is helping patients live longer with acute myeloid leukaemia (AML) — a rare type of cancer that affects the blood and bone marrow. Many patients with AML have recurrent disease within the first two years, even with access to the best available treatment.
By conducting the MRD test, doctors receive advanced warning that the disease is returning several months before the leukaemia is visible under the microscope or the patient develops abnormal blood counts. As soon as MRD was detected to rise, patients were treated with a pill called venetoclax combined with low-dose, under-the-skin injection of chemotherapy that stopped the leukaemia in its tracks in the majority of patients.
Dr Ing-Soo Tiong, a haematologist and researcher at Peter Mac, said with the previous approach to treatment, the median survival after first relapse is only 6–8 months. The new clinical trial results, published in the Journal of Clinical Oncology, show that 50–70% of AML patients are still alive after two years.
“Prior to this discovery, patients and clinicians face the uncertainty of disease relapse, and the only treatment option then was an even stronger dose of salvage chemotherapy requiring at least a month of stay in hospital associated with a very high risk of infection,” Tiong said.
“In this new study, we measured a patient’s MRD as soon as they finished chemotherapy, with the aim of the data telling us which patients were most likely to relapse.”
Professor Andrew Wei, co-lead of the AML program at Peter Mac and The Royal Melbourne Hospital, said this option meant patients could be treated as an outpatient or in the home, with results comparable to intensive chemotherapy.
“This is a paradigm-changing clinical trial that utilises molecular technologies to enable patients to receive their interventional therapy much earlier than normal and with less toxicity,” he said.
“The response to treatment was fast and durable, enabling patients to receive a subsequent stem cell transplant with much lower levels of disease burden and enhanced fitness.
“This is the first ever prospective trial using a pre-emptive MRD-targeted approach,” Wei continued. It has also led to the development of a national trial called INTERCEPT, coordinated by the Australasian Leukaemia and Lymphoma Group, which is currently recruiting patients at Peter Mac and approximately 15 sites nationwide.
ADHD may be linked with an increased risk of dementia
An adult brain affected by attention deficit hyperactivity disorder (ADHD) presents modifications...
Placebos appear to reduce PMS symptoms
Women affected by premenstrual syndrome (PMS) appear to experience less intense and debilitating...
Medicinal cannabis linked to long-term health benefits
As scientists find a way to improve the effectiveness of CBD, a separate study shows that...




