Algorithm helps optimise culture conditions for cell therapy
Cellular therapy is a powerful strategy to produce patient-specific, personalised cells to treat many diseases, including heart disease and neurological disorders — but a major challenge for cell therapy applications is keeping cells alive and well in the lab. Now researchers at Duke-NUS Medical School and Monash University have devised a computational biology algorithm that can predict what molecules are needed to keep cells healthy in laboratory cultures, as described in the journal Cell Systems.
In the laboratory, cells are often grown and maintained in cell cultures formed of a substance called a medium, which contains nutrients and other molecules. It has been an ongoing challenge to identify the necessary molecules to maintain high-quality cells in culture, as well as finding molecules that can induce stem cells to convert to other cell types.
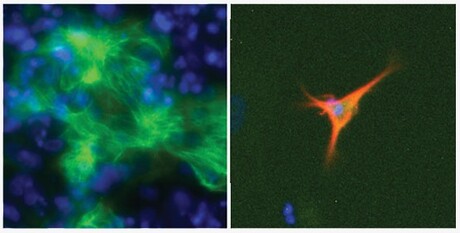
The research team developed a computational approach called EpiMogrify, which can predict the molecules needed to signal stem cells to change into specific tissue cells — and help accelerate treatments that require growing patient cells in the lab. EpiMogrify successfully identified molecules to add to cell culture media to maintain healthy nerve cells, called astrocytes, and heart cells, called cardiomyocytes. The team also used their model to successfully predict molecules that trigger stem cells to turn into astrocytes and cardiomyocytes.
“Computational biology is rapidly becoming a key enabler in cell therapy, providing a way to short-circuit otherwise expensive and time-consuming discovery approaches with cleverly designed algorithms,” said Assistant Professor Owen Rackham, a computational biologist at Duke-NUS and a senior and corresponding author on the study.
The researchers added existing information into their model about genes tagged with epigenetic markers whose presence indicates that a gene is important for cell identity. The model then determines which of these genes actually code for proteins necessary for a cell’s identity. Additionally, the model incorporates data about proteins that bind to cell receptors to influence their activities. Together, this information is used by the computer model to predict specific proteins that will influence different cells’ identities.
“This approach facilitates the identification of the optimum cell culture conditions for converting cells and also for growing the high-quality cells required for cell therapy applications,” said Monash Professor Jose Polo, a senior and corresponding author on the study.
The team compared cultures using protein molecules predicted by EpiMogrify to a type of commonly used cell culture that uses a large amount of unknown or undefined complex molecules and chemicals. They found the EpiMogrify-predicted cultures worked as well or even surpassed their effectiveness.
“The developed technology can identify cell culture conditions required to manipulate cell fate and this facilitates growing important cells in chemically defined cultures for cell therapy applications,” said lead author Dr Uma S Kamaraj, a graduate of Duke-NUS’s Integrated Biology and Medicine PhD Programme.
The researchers have filed for a patent on their computational approach and the cell culture factors it predicted for maintaining and controlling cell fate. EpiMogrify’s predicted molecules are now available for other researchers to explore on a public database: http://epimogrify.ddnetbio.com.
“We aim to continue to develop tools and technologies that can enable cell therapies and bring them to the clinic as efficiently and safely as possible,” Asst Prof Rackham said.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Omega-3s appear to slow down the aging process
Researchers have found that taking omega-3 fatty acids slows down biological aging across several...
Stress during pregnancy could affect the baby's development
Maternal stress could leave epigenetic imprints on genes in the placenta associated with...
Bird flu detected at Victorian poultry farm
Agriculture Victoria has confirmed the presence of avian influenza at a poultry property in...



