Autoantibodies cause lifelong susceptibility to viral infections
Swiss researchers have found that about 2% of the population develop autoantibodies against type 1 interferons, mostly later in life, which makes individuals more susceptible to viral diseases like COVID-19. Their work has been published in the Journal of Experimental Medicine.
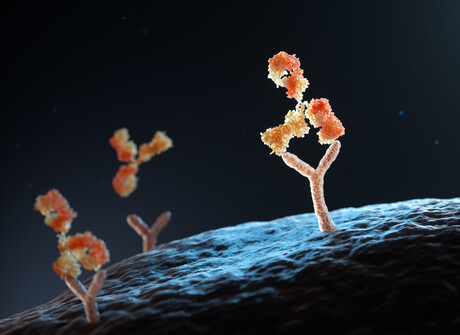
Virus infections trigger the cells of the immune system to release type 1 interferons, which act as early messengers that warn uninfected cells and tissues that a virus is spreading. But in individuals with a compromised type 1 interferon system, severe viral infections can occur because the body cannot mount a full defence. Indeed, recent research has shown that 5–15% of people who are in hospital with severe COVID-19 or influenza have a deficiency in their type 1 interferon response, because their blood contains autoantibodies — antibodies that target a person’s own structures — that bind type 1 interferons and stop the messenger from functioning.
Professor Benjamin Hale and his team at the University of Zurich (UZH) wanted to find out the cause, as well as the consequences, of some people having autoantibodies against type 1 interferons. In order to do this, they utilised the frozen blood samples of around 2000 adults who had donated samples twice a year for several decades as part of the Swiss HIV Cohort Study (the fact that the donors had HIV had no relevance for the results, as in this cohort the virus was suppressed by treatment).
First, the team analysed the blood samples for the presence of autoantibodies against type 1 interferons. This analysis revealed that around 2% of individuals produced autoantibodies against type 1 interferons in their lifetime and that this typically occurred between the ages of 60 to 65. This confirms prior studies that reported that the prevalence of autoantibodies against type 1 interferons might increase with age.
Next, by studying clinical data, researchers at the University Hospital Zurich (USZ) were able to understand which factors contributed to the development of autoantibodies against type 1 interferons. The individuals who developed them appeared to be prone to also producing antibodies against other proteins formed by their own bodies. This so-called loss of self-tolerance can occur in some people as they age.
“These individuals may produce antibodies against their own type 1 interferons because they are both prone to making autoantibodies and are exposed to high levels of type 1 interferons, for example because their immune system produces interferons against other infections at the time,” Hale said.
Importantly, the study found that, once developed, these autoantibodies remained detectable in the blood of individuals for the rest of their lives. People with autoantibodies against type 1 interferons, even when they had developed them as far back as in 2008, were more likely to suffer from severe COVID-19 in 2020. These autoantibodies thus had consequences for individuals decades later, leading to a compromised type 1 interferon system and reduced immunity against viruses.
Understanding these risk factors might lead to future diagnostic tests that can identify older individuals who are more prone to developing this deficiency, and therefore help with measures to prevent autoantibodies ever developing. Identifying individuals with autoantibodies against type 1 interferons could also help to prioritise these people for vaccines or antivirals to prevent severe viral infections.
SEQ koala population carries immunity to retrovirus
Koalas from a population north of the Brisbane River appear to have evolved a unique genomic...
RSV immunisation program for babies slashes hospital stays
An Australian-first study has demonstrated the effectiveness of immunisation against respiratory...
A targeted treatment option for psoriasis
New research from MedUni Vienna paves the way for the development of a therapy that not only...




