Breast cancer cells turned into fat cells in mice
Swiss researchers have developed an innovative combination therapy that can force malignant breast cancer cells to turn into fat cells, which can be used to prevent the formation of metastases in mice. Their work has been reported in the journal Cancer Cell.
Tumour cells can adapt dynamically to changing conditions thanks to their ability to reactivate a cellular process that is central to embryonic development, known as epithelial–mesenchymal transition (EMT). While EMT is used by stem cells to differentiate into a variety of cell types throughout the body, and for tissue regeneration such as wound healing, it can also be exploited by tumour cells looking to leave the primary tumour, enabling them to spread around the body and form metastases in distant organs.
The good news is that cells undergoing EMT are in a highly changeable state, providing a window of opportunity for therapeutic targeting. With this in mind, scientists from the University of Basel’s Department of Biomedicine, led by Professor Gerhard Christofori, have been researching the molecular processes that regulate the cellular EMT program, developing a new therapeutic approach to tumour treatment in the process.
The researchers tested their approach in mouse models for metastatic breast cancer, created by transplanting human breast cancer cells into the mammary fat pad of female mice. The mice were dosed with a combination of two FDA-approved drugs: Rosiglitazone, which is widely used to treat patients with diabetes, and Trametinib, which inhibits the growth and spread of cancer cells.
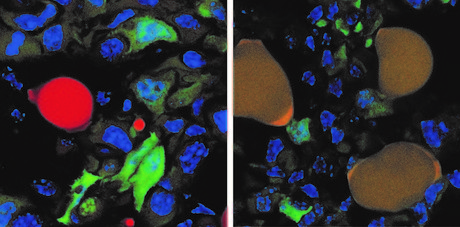
It did not take long for the mice’s breast cancer cells — which usually divide quickly and form metastases — to be converted into fat cells that can no longer divide and can barely be differentiated from normal fat cells. In particular, the researchers targeted a handful of aggressive cancer cells that had left the primary tumour and invaded surrounding tissue. These cells were readily converted to fat cells, while the remaining cancer cells within the tumour were no longer able to proliferate unchecked.
“The breast cancer cells that underwent an EMT not only differentiated into fat cells, but also completely stopped proliferating,” Professor Christofori said. The drugs also suppressed the growth of primary tumours in the mice and prevented the tumours from metastasising throughout the animals’ bodies.
“As far as we can tell from long-term culture experiments, the cancer cells-turned-fat cells remain fat cells and do not revert back to breast cancer cells.”
The researchers hypothesise that forcing a critical mass of cancerous cells to differentiate into fat cells could deplete a tumour’s ability to fight off conventional chemotherapy. Next steps involve testing the EMT-targeted differentiation approach in combination with existing chemotherapies and in other types of cancers.
“In future, this innovative therapeutic approach could be used in combination with conventional chemotherapy to suppress both primary tumour growth and the formation of deadly metastases,” Professor Christofori said.
Follow us on Twitter and Facebook for the latest industry news. To receive our bimonthly magazine and weekly newsletters, click here.
Damaged RNA, not DNA, revealed as main cause of acute sunburn
Sunburn has traditionally been attributed to UV-induced DNA damage, but it turns out that this is...
Multi-ethnic studies identify new genes for depression
Two international studies have revealed hundreds of previously unknown genetic links to...
Oxygen deprivation may contribute to male infertility
Medical conditions that deprive the testes of oxygen, such as sleep apnoea, may be contributing...



