Faecal microbial transplantation treats C. diff infection
An innovative treatment for patients with Clostridium difficile infection (CDI), which uses transplanted gut bacteria to treat the infection, has been shown to be a more effective and more cost-efficient treatment than using antibiotics.
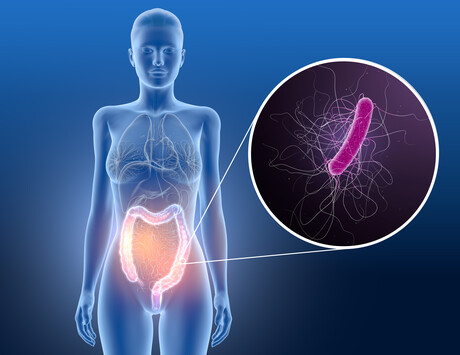
CDI is an infection of the bowel that commonly affects people who have recently been treated in hospital, those with underlying conditions and patients over 65. Almost 30% of patients treated for the condition experience at least one recurrence, which is usually treated using antibiotics.
Faecal microbial transplantation (FMT), a treatment pioneered as a licensed medicine by Professor Peter Hawkey and his team at the University of Birmingham, is a method where gut bacteria and other components in faeces are used to treat CDI. The bacteria is taken from a screened healthy donor, processed and screened before being transplanted via a tube passed through the nose into the stomach.
Treatment with FMT is associated with higher cure and lower recurrence rates than fidaxomicin or vancomycin — the two most common antibiotics used to treat recurrent CDI (rCDI) — but Birmingham researchers wanted to analyse all options in terms of treatment effects, unit costs, resources and health-related quality of life to identify which treatment was the most cost-effective and offered the best outcome for patients. The team analysed randomised controlled trials and observational studies on hospitalised patients with single or multiple rCDI, with the results of their study published in the journal EClinicalMedicine.
The study showed that both methods for administering FMT were lower in cost compared to standard treatment with antibiotics. FMT via naso-gastric tube was the least costly, with a mean cost of £8877 per patient, while FMT via colonoscopy was £11,716 per patient. FMT via colonoscopy was also shown to be slightly more effective than treatment via naso-gastric tube, offering patients a higher quality of life. Both vancomycin and fidaxomicin were shown to be more costly and less effective than either of the FMT interventions; moreover, vancomycin was the most expensive and the least effective treatment.
Professor Tracy Roberts, Head of the University of Birmingham’s Health Economics Unit, said, “As well as being more effective both in terms of cost and benefit to patients, FMT was shown to significantly reduce the amount of days patients were required to be hospitalised, which could also provide longer term cost savings.”
Prof Hawkey concluded, “We at the University of Birmingham pioneered this treatment as the UK’s first third-party FMT service. FMT is not currently a widespread treatment for this disease but, by showing that it not only saves lives but is also significantly more cost-effective, we hope that this could be one of the first steps towards the treatment being accepted more widely.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Pancreatic cancer hijacks metabolism switch to help it spread
Pancreatic cancer hijacks a molecule known for regulating physiological processes, such as food...
Novel antibiotic activates 'suicide' mechanism in superbug
Researchers have discovered a new class of antibiotic that selectively targets Neisseria...
Modifications in the placenta linked to psychiatric disorders
Schizophrenia, bipolar disorder and major depression disorder are the neuropsychiatric disorders...




