Functional pancreatic beta cells produced from stem cells
Researchers from the University of Helsinki and Uppsala University have found a way to optimise the functionality of pancreatic cells produced from stem cells, paving the way for cell therapies for diabetes. Their breakthrough has been published in the journal Nature Biotechnology.
Insulin is a vital hormone produced by pancreatic beta cells. Type 1 diabetes is caused by the destruction of these cells, which results in patients having to replace the lost insulin with multiple daily injections. Insulin secretion can be restored in diabetic patients by transplanting beta cells isolated from the pancreas of a brain dead organ donor; however, this treatment has not been widely introduced, since cells from at least two donors are needed to cure one diabetic.
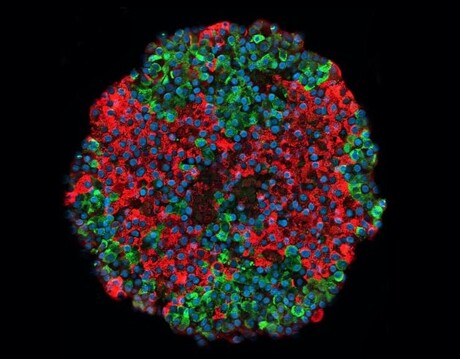
For a long time, attempts have been made to produce functional beta cells from stem cells, which could make this treatment increasingly common. However, the beta cells produced from stem cells have so far been immature, with poorly regulated insulin secretion. A research group headed by Professor Timo Otonkoski, from the University of Helsinki, has now demonstrated that stem cells can form cells that closely mimic normal pancreatic islets, in terms of both structure and function.
“In our study, insulin secretion was regulated as usual in cells, and the cells responded to changes in the glucose level even better than the pancreatic islets isolated from organ donors that were used as controls,” said Helsinki’s Väinö Lithovius, a member of the research group.
The researchers demonstrated the function of stem cell-derived beta cells in both cell cultures and mice studies. In the latter, the researchers demonstrated that stem cell-derived beta cells transplanted into mice started effectively managing the glucose metabolism of the mice.
“Blood glucose levels are higher in mice than in humans, roughly 8–10 mM,” said Helsinki researcher Jonna Saarimäki-Vire, who was responsible for the cell transplantation. “After the cell transplantation, the level decreased to that seen in humans, roughly 4–5 mM. It remained at this level, proving that the stem cell-derived transplant was capable of regulating blood glucose levels in mice.”
In addition to insulin secretion, the researchers investigated the functionality of systems that regulate insulin secretion, including metabolism and ion channels, also connecting the findings to gene expression occurring during development.
“Our study will help further improve the production of stem cell islets, which will make it easier to utilise them in disease modelling and cell therapies,” Prof Otonkoski said.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
ADHD may be linked with an increased risk of dementia
An adult brain affected by attention deficit hyperactivity disorder (ADHD) presents modifications...
Placebos appear to reduce PMS symptoms
Women affected by premenstrual syndrome (PMS) appear to experience less intense and debilitating...
Medicinal cannabis linked to long-term health benefits
As scientists find a way to improve the effectiveness of CBD, a separate study shows that...




