Fungal infection's deadly transformation uncovered
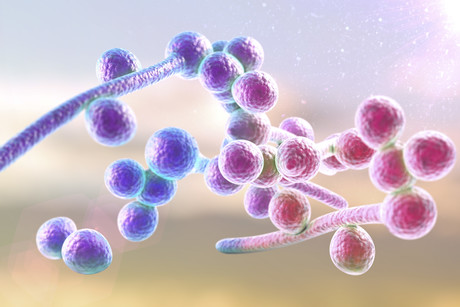
Monash University scientists have shed light on how the fungal infection Candida albicans transforms into a deadly version with hyphae or filaments that help it break through human tissues and into the bloodstream. Published in the journal Cell Reports, their research could be key to the development of drugs against this fatal infection.
Fungal infections, such as those from C. albicans, are a common form of bloodstream infections in hospitals, particularly in very sick or immunocompromised patients. They can also lead to sepsis-like disease. Fungi cause untold harm — with estimated mortality rates of 10–20% — largely because they are so similar to mammalian cells that few antifungal therapies are available. There is also no sure-fire way to treat or prevent C. albicans infections and, as the population living with weakened immune systems (including HIV and transplant patients, those undergoing chemotherapy and preterm babies) increases, the threat of this fungus is growing.
Although C. albicans lives in the gut of about half of all people, it has an ability to transform into a form in which it can invade tissues and also escape from immune cells. In the gut, C. albicans sits in a benign state until the right opportunity occurs, when it can overgrow and also start to form hyphae or filaments. These filaments are elongated, stick-shaped cells that the yeast can use to push through the gut wall and get access to the bloodstream and organs, so that it can spread its infection.
Researchers from the Monash Biomedicine Discovery Institute, led by Associate Professor Ana Traven, have now shed light on how C. albicans shapeshifts to the deadly hyphal version. Understanding this process is a major breakthrough, building the knowledge base that could lead to development of drugs to treat this infection.
The study focuses on the compound mdivi-1, which is generating global interest in preclinical studies of non-infectious human diseases such as neurodegenerative conditions, stroke, heart attack and cancer. According to Assoc Prof Traven, to her knowledge the compound has not been studied extensively in the context of infectious diseases.
In laboratory studies, the team found that adding mdivi-1 to the culture medium inhibits the transition to the hyphal form of the fungus. The researchers used the ability to halt this process to study just how the transition happens at a molecular level.
“We revealed a mechanism that operates in C. albicans cells to promote hyphal switching via a molecule called nitric oxide, opening a new avenue for understanding this key process and potentially leading to development of new antifungal drugs in the future,” Assoc Prof Traven said.
“The mortality rate for bloodstream Candida infections is substantial even in countries where the best care is available, so a potential new therapeutic route is very important.”
Follow us on Twitter and Facebook for the latest industry news. To receive our bimonthly magazine and weekly newsletters, click here.
Archer completes potassium sensing alpha prototype
Quantum technology company Archer Materials Limited has developed an early Biochip prototype...
Farm animals and aquaculture cryopreservation partnership announced
Vitrafy Life Sciences Limited has announced that it has entered a 12-month exclusive agreement...
Babies of stressed mothers likely to get their teeth earlier
Maternal stress during pregnancy can speed up the timing of teeth eruption, which may be an early...



