Gene therapy for frontotemporal dementia
A new therapeutic approach for treating frontotemporal dementia — an incurable brain disease causing memory loss, speech disorders and changes in personality — uses modified viruses to replace a missing protein in the brain. The method has been described in the journal Science Translational Medicine.
In 5–12% of cases, frontotemporal dementia is triggered by a decline in progranulin. The loss of this protein leads to deficiencies in protein breakdown, resulting in the deposition of insoluble toxic proteins. This leads to inflammation of the brain, neuronal death and associated massive functional disorders of the central nervous system. Researchers at LMU Munich and the German Center for Neurodegenerative Diseases (DZNE), working in close cooperation with Denali Therapeutics, have now developed a therapeutic approach that makes it possible to replace the missing protein in the brain.
“We inserted progranulin into the genome of a virus,” explained Dr Anja Capell, a senior scientist at LMU’s Biomedical Center and a lead author on the study. Next, the team injected the modified viruses into the bloodstream of mouse models.
“The virus targeted liver cells, which then produce progranulin in large quantities and release it into the blood,” Capell continued. In this way, the approach avoids injecting viruses directly into the brain, with the associated risk of major side effects.
To get this peripheral solution to work, the researchers had to use a trick to get past the blood–brain barrier, which usually blocks the exchange of biomolecules between blood and brain. A so-called brain shuttle, developed by Denali Therapeutics, permits effective transport across this barrier.
“After administering the virus once, we checked whether the symptoms were reduced,” said co-lead author Professor Dominik Paquet, from LMU Munich’s Institute for Stroke and Dementia Research (ISD). It turned out that deficits in protein degradation, the deposition of insoluble toxic proteins, inflammation of the brain, movement disorders and the death of neurons were all massively reduced.
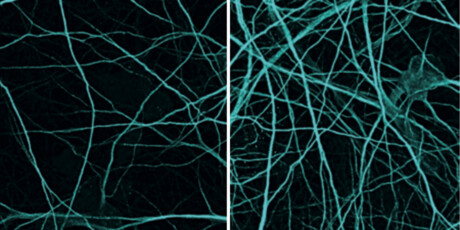
“As the next step, we investigated in stem cell models whether this approach can be transferred to humans,” Paquet said. Here, too, there was a significant reduction in symptoms of the disease.
Through this approach, the researchers were able to demonstrate that forms of frontotemporal dementia that are based on a partial loss of progranulin are treatable in preclinical trials using a replacement therapy. Principal investigator Professor Christian Haass, from the LMU Biomedical Center, added, “This study also shows the importance of intensifying our collaboration with leading biotech companies so that we can bring our research to clinical practice as rapidly as possible for the benefit of patients.”
Novel antibiotic activates 'suicide' mechanism in superbug
Researchers have discovered a new class of antibiotic that selectively targets Neisseria...
Modifications in the placenta linked to psychiatric disorders
Schizophrenia, bipolar disorder and major depression disorder are the neuropsychiatric disorders...
ADHD may be linked with an increased risk of dementia
An adult brain affected by attention deficit hyperactivity disorder (ADHD) presents modifications...




