High BMI negatively impacts brain function
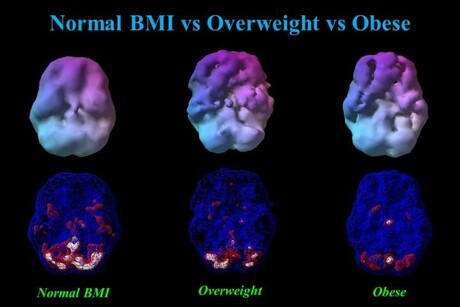
As a person’s weight goes up, all regions of the brain go down in activity and blood flow. That’s according to a new brain imaging study — one of the largest to link obesity with brain dysfunction — published in the Journal of Alzheimer’s Disease.
Led by Dr Daniel G Amen, founder of Amen Clinics in the US, scientists analysed over 35,000 functional neuroimaging scans using single-photon emission computerised tomography (SPECT) from more than 17,000 individuals to measure blood flow and brain activity. Low cerebral blood flow is the number one brain imaging predictor that a person will develop Alzheimer’s disease, and is also associated with depression, ADHD, bipolar disorder, schizophrenia, traumatic brain injury, addiction, suicide and other conditions.
Striking patterns of progressively reduced blood flow were found in virtually all regions of the brain across categories of underweight, normal weight, overweight, obesity and morbid obesity. In particular, brain areas noted to be vulnerable to Alzheimer’s disease — the temporal and parietal lobes, hippocampus, posterior cingulate gyrus and precuneus — were found to have reduced blood flow along the spectrum of weight classification from normal weight to overweight, obese and morbidly obese.

The study thus shows that being overweight or obese seriously impacts brain activity and increases the risk for Alzheimer’s disease as well as many other psychiatric and cognitive conditions, Dr Amen said. It also highlights the need to address obesity as a target for interventions designed to improve brain function, be they Alzheimer’s disease prevention initiatives or attempts to optimise cognition in younger populations.
“One of the most important lessons we have learned through 30 years of performing functional brain imaging studies is that brains can be improved when you put them in a healing environment by adopting brain-healthy habits, such as a healthy calorie-smart diet and regular exercise,” Dr Amen said.
Dr George Perry, Editor-in-Chief of the Journal of Alzheimer’s Disease, concluded, “Acceptance that Alzheimer’s disease is a lifestyle disease, little different from other age-related diseases … is the most important breakthrough of the decade. Dr Amen and collaborators provide compelling evidence that obesity alters blood supply to the brain to shrink the brain and promote Alzheimer’s disease. This is a major advance because it directly demonstrates how the brain responds to our body.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Novel antibiotic activates 'suicide' mechanism in superbug
Researchers have discovered a new class of antibiotic that selectively targets Neisseria...
Modifications in the placenta linked to psychiatric disorders
Schizophrenia, bipolar disorder and major depression disorder are the neuropsychiatric disorders...
ADHD may be linked with an increased risk of dementia
An adult brain affected by attention deficit hyperactivity disorder (ADHD) presents modifications...




