How immune cells communicate across the blood–brain barrier
Australian and US immunologists have broken ground with new knowledge into how cells communicate across the brain’s protective blood–brain barrier — a breakthrough that could change the way researchers look at diseases such as malaria, multiple sclerosis and Alzheimer’s.
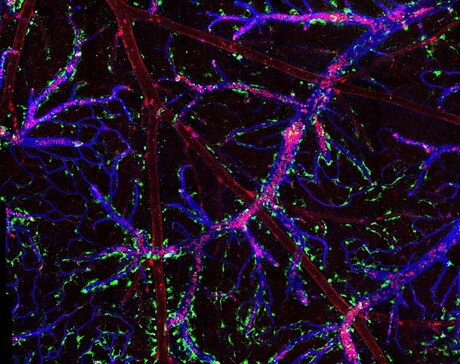
The scientists developed a high-tech laser microscopy imaging model, which has given them a rare peek inside blood vessels to watch immune cell behaviour in real time. Dr Saparna Pai, from the Australian Institute of Tropical Health and Medicine at James Cook University, said what they found could change the current understanding of what happens in patients with deadly diseases such as malaria.
“There has been a gap in our knowledge of how immune cells promote diseases of the nervous system such as cerebral malaria,” Dr Pai said. “What we saw was a group of immune cells called T cells driving inflammation in the brain, and we found they don’t act alone: they need a licence to kill.
“We now know they are guided by another specialised cell known as perivascular macrophages (PVM), which we saw guiding the T cells across the blood vessel, through the blood–brain barrier, into the brain.
“We discovered these specialised immune cells known as PVM, which line the outer wall of blood vessels, may actively communicate with circulating T cells, leading to inflammation of the brain and death, during cerebral malaria.”
In a patient with cerebral malaria, the red blood cells become ‘sticky’, blood flow becomes sluggish and the endothelium membrane lining the blood vessels also becomes inflamed. Recently, US researchers found T cells also get stuck to the endothelium membrane and were able to find their way into the brain.
Existing medical understanding is that this membrane lining the blood vessel is what attracts and assists the T cells to cross the blood–brain barrier. But the latest research, published in the journal Clinical & Translational Immunology, shows that PVM play an important role.
“Several studies have demonstrated the indispensable role of these T cells in the development of cerebral malaria, but their precise activities within the brain that contribute to neurological disease were only recently documented by our group,” Dr Pai said.
“PVM cells communicating with T cells across the blood–brain barrier is a highly innovative concept that has not been previously identified. If these findings are validated, they may provide a new therapeutic target for the treatment of several diseases in which PVM play a crucial role in disease progression.”
These diseases include multiple sclerosis, where the T cells cross the blood–brain barrier and find their way into the second layer of brain tissue, and may also have implications for the prevention and treatment of diseases such as Alzheimer’s and viral encephalitis.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Damaged RNA, not DNA, revealed as main cause of acute sunburn
Sunburn has traditionally been attributed to UV-induced DNA damage, but it turns out that this is...
Multi-ethnic studies identify new genes for depression
Two international studies have revealed hundreds of previously unknown genetic links to...
Oxygen deprivation may contribute to male infertility
Medical conditions that deprive the testes of oxygen, such as sleep apnoea, may be contributing...



