Immune cells in the brain can cooperate when needed
To break down toxic proteins more quickly, immune cells in the brain can join together to form networks when needed. However, in certain mutations that can cause Parkinson’s disease, this cooperation is impaired.
That’s the conclusion of a new study from the University of Bonn, the German Center for Neurodegenerative Diseases (DZNE) and the François Jacob Institute of Biology. The research team’s findings have been published in the journal Cell.
The protein alpha-synuclein (aSyn) performs important tasks in the nerve cells of the brain. But under certain circumstances, aSyn molecules can clump together and form insoluble aggregates. These damage the neurons; they are for instance typically found in the brains of people suffering from Parkinson’s disease or Lewy body dementia. The immune cells of the brain, the microglial cells, therefore try to break down and dispose of the aSyn aggregates — a process that is not only time-consuming but can also cause the microglial cells themselves to perish.
“We have now identified a mechanism that addresses both problems,” said Prof Dr Michael Heneka, who conducts research at the University Hospital Bonn and DNZE on neurodegenerative diseases such as Parkinson’s and Alzheimer’s disease.
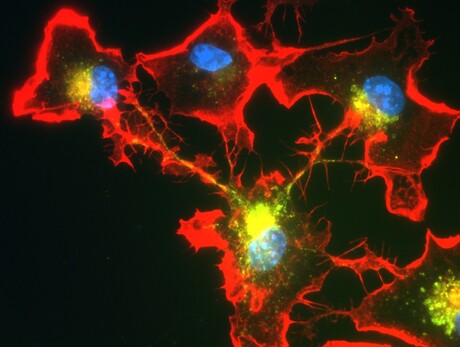
Prof Dr Heneka and his team have found that microglial cells may spontaneously join together in order to better cope with threats. For this purpose, they form tube-like projections that dock onto neighbouring microglial cells. These connections are then used to distribute the aSyn aggregates among the partners in the network. Without this division of labour, individual immune cells would have to shoulder a major part of the degradation work and would be overwhelmed. Joining forces prevents that from happening.
The connecting tubes also serve another purpose: microglial cells can use them to give their neighbours a boost when they are in too much distress or indeed in mortal danger. “They then send mitochondria to neighbouring cells that are busy breaking down the aggregates,” explained Dr Hannah Scheiblich, a colleague of Prof Dr Heneka. “Mitochondria function like little power plants, so they provide extra energy to the stressed cells.”
In certain mutations, which are found more frequently in Parkinson’s disease patients, both aSyn and mitochondrial transport are impaired. A similar situation applies to another disease in which the degradation of aSyn is impaired: Lewy body dementia. The researchers isolated certain immune cells, the macrophages, from the blood samples of affected individuals; these were converted into microglia-like cells with the help of specific regulatory molecules.
“These were still able to form networks in the lab; however, the transport of aSyn through the connecting tubes was severely impaired,” Prof Dr Heneka said.
The fact that microglial cells can join together was previously unknown, and may open up new therapeutic perspectives for neurological disorders such as Parkinson’s disease or dementia.
“We have opened the door to a field that will certainly engage researchers for many years to come,” Prof Dr Heneka said.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Damaged RNA, not DNA, revealed as main cause of acute sunburn
Sunburn has traditionally been attributed to UV-induced DNA damage, but it turns out that this is...
Multi-ethnic studies identify new genes for depression
Two international studies have revealed hundreds of previously unknown genetic links to...
Oxygen deprivation may contribute to male infertility
Medical conditions that deprive the testes of oxygen, such as sleep apnoea, may be contributing...



