Ineffective psoriasis drugs block the wrong mechanism
Just in time for World Psoriasis Day (29 October), a day dedicated to spreading awareness of psoriasis and psoriatic disease, researchers from the University of Zurich (UZH) have published a study explaining why common psoriasis drugs show insufficient treatment efficacy.
Psoriasis is a chronic inflammatory autoimmune disease that manifests as red, scaly skin patches. There is no causal treatment for the disease, but the symptoms can be significantly alleviated with modern therapies. Interleukin-12 — a messenger molecule of immune cells — was long considered to trigger the development of psoriasis, but UZH researchers have now discovered this is not the case.
Complex changes in the networks of immune cells and the messengers they use to communicate with each other are responsible for the development of psoriasis. Clinical trials had revealed that newly developed drugs blocking only the messenger interleukin-23 are more effective than previous treatments targeting both interleukin-23 and interleukin-12 in psoriasis patients. The responsible mechanism has so far remained unknown.
The research teams of Professor Burkhard Becher and Sarah Mundt from UZH have systematically investigated the function of interleukin-12 in psoriasis. Their study, published in the journal Science Immunology, shows that the messenger does not contribute to the disease — on the contrary, it protects against it.
“These results surprised us,” Prof Becher said, “because so far drugs for the treatment of psoriasis also aim at blocking interleukin-12.”
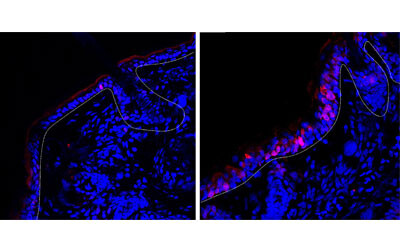
Detailed studies in mice and with human tissue have shown that various cell types in the skin are also equipped with receptors for interleukin-12. This means the messenger can be recognised not only by the T cells of the immune system, but also keratinocytes — horn-forming skin cells that build up the epidermis. In fact, the recognition of interleukin-12 by these skin cells was responsible for the protective effect of the messenger, as the researchers found out.
“Interleukin-12 is essential for the normal, physiological function of keratinocytes,” Mundt said. “For example, it prevents the increased cell division observed in psoriasis.”
“Our findings indicate that blocking interleukin-12 is not advisable, and such drugs should therefore no longer be used to treat psoriasis patients,” added Pascale Zwicky, PhD student and first author of the study. Accordingly, psoriasis drugs should only block the messenger substance interleukin-23, but no longer interleukin-23 and -12 together.
The researchers’ findings could also be important for the treatment of other diseases, with Prof Becher noting, “The combined blocking of interleukin-23 and -12 is also used in the treatment of chronic inflammatory bowel diseases and psoriatic arthritis. In these diseases, the role of interleukin-12 has not yet been sufficiently studied. But here, too, a protective role of the messenger substance is possible.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Babies of stressed mothers likely to get their teeth earlier
Maternal stress during pregnancy can speed up the timing of teeth eruption, which may be an early...
Customised immune cells used to fight brain cancer
Researchers have developed CAR-T cells — ie, genetically modified immune cells manufactured...
Elevated blood protein levels predict mortality
Proteins that play key roles in the development of diseases such as cancer and inflammation may...




