Pancreas-on-a-chip could help cystic fibrosis patients
Scientists from the Cincinnati Children’s Hospital Medical Center have created a human pancreas-on-a-chip — a small, two-chambered device featuring bioengineered human pancreatic organoids — that allowed them to identify the possible cause of a frequent and deadly complication of cystic fibrosis called CF-related diabetes (CFRD). Their research has been published in the journal Nature Communications.
The device was created to help people with cystic fibrosis (CF) — a genetic lung disease caused by a mutation in the CFTR gene that leads to a water and salt imbalance on cell surfaces and clogs the lungs with thick mucus. Although mutations in the CFTR gene are known to cause cystic fibrosis, its role in CFRD is unclear, and until now there hasn’t been an effective way to study CFRD in the lab.
“Mouse models of CF don’t faithfully re-create CF-related diabetes in the lab, and it wasn’t possible to study the disease at the depth we achieved in this study,” said Dr Anjaparavanda Naren, principal investigator on the study.
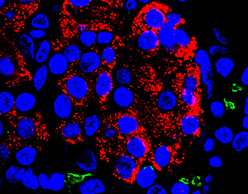
The researchers started by isolating pancreatic ductal epithelial cells and pancreatic islets donated by surgical patients. The ductal organoids were cultured in a transparent dual chamber called a microfluidic device, which contained specific biochemical solutions to generate the pancreas-on-a-chip. Ductal epithelial cells were cultured in the top chamber and pancreatic islet cells were in the bottom chamber, separated by a thin layer of porous membrane that allowed the different chambers to interact. The cells grew and expanded into three-dimensional pancreatic organs that mimicked cell-to-cell communications and fluid exchange, similar to the function of a naturally developed human pancreas.

When the researchers tested their pancreas-on-a-chip by disrupting CFTR gene expression, it impaired cell-to-cell communication and fluid exchange and negatively affected endocrine function. This caused an insulin deficiency and re-created the CFRD disease process. The researchers said this confirmed that the CFTR gene has a direct role in regulating insulin secretion and causing diabetes in people with CF.
The in vitro chip technology can be used to study CFRD and glucose imbalance in specific individuals with the condition, creating the potential for diagnosing different disease manifestations on a highly personalised basis. It can help assay variability in the glucose measures of different people, determine correlation of glucose levels with the CFTR mutation type and test small-molecule interventions.
“Our technology closely resembles the human pancreas and potentially may help us find therapeutic measures to manage glucose imbalance in people with CF, which is linked to increased illness and death,” Dr Naren said.
The research team now plans to use the device in a pilot study to test FDA-approved drugs that modulate CFTR gene expression, with the aim of determining how well different CFTR drugs can slow or reverse lab-simulated CFRD. The device could also potentially be used to study the causes of non-CF-related conditions such as type 1 and 2 diabetes, the researchers said.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Quitting smoking increases life expectancy even for seniors
Although the benefits of quitting smoking diminish with age, there are still substantial gains...
Stem cell transplants treat blindness in mini pigs
Scientists have successfully transplanted retinas made from stem cells into blind mini pigs,...
Sugary drinks raise cardiovascular disease risk, but occasional sweets don't
Although higher sugar intake raises your risk of certain cardiovascular diseases, consuming sweet...





