Two new methods for faster sepsis diagnosis
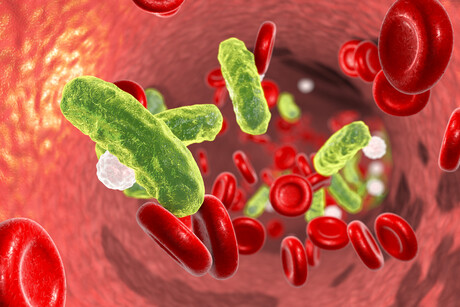
Sepsis and septic shock patients could soon experience faster diagnoses and better outcomes, with blood plasma metabolic phenotyping having been successfully used to accurately diagnose the conditions within one hour of blood collection. This is in comparison to the current testing method — pathogen culturing — which can take days to confirm.
Sepsis is a life-threatening condition where the body has an extreme response to an infection, causing organ damage. As noted by Dr Sam Lodge, from Murdoch University’s Australian National Phenome Centre, “It needs immediate medical attention, or it can cause death or permanent damage to your body.
“A timely diagnosis has the potential to significantly reduce mortality rates.”
In a study led by Murdoch University, blood plasma samples were collected from 152 ICU patients in Western Australian hospitals. Using 15 identified parameters, consisting of various metabolites, lipids, lipoproteins and inflammatory markers, patients were able to be quickly placed into the correct clinical outcome, as documented in the Journal of Proteome Research.
“We found that non-sepsis, sepsis and septic shock intensive care unit (ICU) patients have differential metabolic signatures, which can be used to diagnose patients quickly — within one hour of blood collection,” Lodge said.
Patients with sepsis or septic shock exhibited higher concentrations of neopterin and lower levels of HDL cholesterol and phospholipid particles in comparison to non-sepsis patients. Septic shock patients could be differentiated from sepsis patients based on different concentrations of 10 lipids.
“While further validation with a larger cohort is required, this study provides a proof of concept for the potential use of metabolic phenotypes in better diagnosing these conditions,” Lodge said.
The news was announced just two weeks after University of Queensland (UQ) researchers revealed their own method to predict if a child is likely to develop sepsis and go into organ failure. The UQ study, which was published in The Lancet Child & Adolescent Health, involved more than 900 critically ill children in the emergency departments and ICUs of four Queensland hospitals.
“Blood samples were taken from these patients at the acute stage of their infection, and we analysed which genes were activated or deactivated,” said Associate Professor Lachlan Coin, from UQ’s Institute for Molecular Bioscience.
“We were able to identify patterns of gene expression which could predict whether the child would develop organ failure within the next 24 hours, as well as whether the child had a bacterial or viral infection or a non-infectious inflammatory syndrome.”
Professor Luregn Schlapbach, from UQ’s Child Health Research Centre, said diagnosing sepsis in children can be particularly challenging as many paediatric illnesses can present the same, so having precision markers that tell you whether a child is going to develop the condition is urgently needed.
“Currently doctors give antibiotics, fluids and increase observation of any child if sepsis is suspected, but unfortunately that means there are children who receive unnecessary treatment,” he noted. The new study is therefore a big leap forward, although more research will be needed before clinicians can act pre-emptively.
“Our next step will be to transfer what we have discovered to a point-of-care platform, which means we can potentially generate the results from a blood test within an hour,” he said.
A simple finger prick can be used to diagnose Alzheimer's
A new study is paving the way for a more accessible method of Alzheimer's testing, requiring...
Experimental blood test detects early-stage pancreatic cancer
The new test works by detecting two sugars — CA199.STRA and CA19-9 — that are...
Biomarkers for dementia vary with time of day
Biomarkers used to diagnose Alzheimer's, including a promising marker for early diagnosis of...





