Scientists grow genetically modified skin using stem cells
Scientists have reconstructed a fully functional epidermis, covering approximately 80% of the total body surface area, for a seven-year-old boy with a genetic skin disease called Junctional Epidermolysis Bullosa (JEB). The findings are reported in Nature.
JEB is a severe, often lethal, genetic disease that causes the skin to become fragile. Mutations in the genes LAMA3, LAMB3 or LAMC2 affect a protein called laminin-332 — a component of the basement membrane of the epidermis — leading to blistering of the skin and chronic wounds, which impair the patient’s quality of life and can lead to skin cancer.
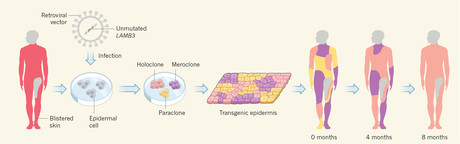
After all established therapies had failed, the medical team from Ruhr University Bochum, Germany, in collaboration with Prof Dr Michele De Luca from the Center for Regenerative Medicine at the University of Modena, opted for an experimental therapy — the transplantation of genetically modified epidermal stem cells. Obtained from the patient via skin biopsy, these stem cells were processed in Modena. The researchers transferred the intact gene into acquired stem cells. During this process, so-called retroviral vectors were deployed, ie, virus particles that had been specifically modified for gene transfer.
The genetically modified stem cells had been cultivated in a clean room laboratory and subsequently turned into transgenic transplants. The transplants were applied to the boy’s arms and legs, entire back, flanks, and partially to the stomach, neck and face as well. “Overall, 0.94 square metres of transgenic epidermis were transplanted onto the young patient in order to cover all defects, accounting for 80% of his entire body surface,” said Associate Professor Dr Tobias Hirsch, Plastic Surgeon from Bochum Children's Hospital.
Over the course of the next 21 months, the regenerated epidermis firmly adhered to the underlying dermis, even after induced mechanical stress, healed normally and did not form blisters.
Through the process of clonal tracing, the authors found that the human epidermis is sustained by a limited number of long-lived stem cells which are able to extensively self-renew and can produce progenitors that replenish terminally differentiated keratinocytes.
Because of its large scale, the case is considered unique on a worldwide level. “Transplanting 80% of the skin and providing intensive medical care to the patient over a period of eight months was extremely challenging,” Tobias Rothoeft and Tobias Hirsch pointed out. “The close collaboration between the departments in Bochum and the University of Modena’s expertise have been the key to success. This makes us very proud.”
Breakthrough blood test for endometriosis developed
Scientists identified 10 protein biomarkers, or 'fingerprints' in the blood, that can be...
A simple finger prick can be used to diagnose Alzheimer's
A new study is paving the way for a more accessible method of Alzheimer's testing, requiring...
Experimental blood test detects early-stage pancreatic cancer
The new test works by detecting two sugars — CA199.STRA and CA19-9 — that are...




