Bioengineered ears look and act like the real thing
Physicians at Weill Cornell Medical College and biomedical engineers at Cornell University have succeeded in building a facsimile of a living human ear that looks and acts like a natural ear. They believe their bioengineering method will finally succeed in the long quest by scientists and physicians to provide normal-looking ‘new’ ears to thousands of children born with a congenital ear deformity.
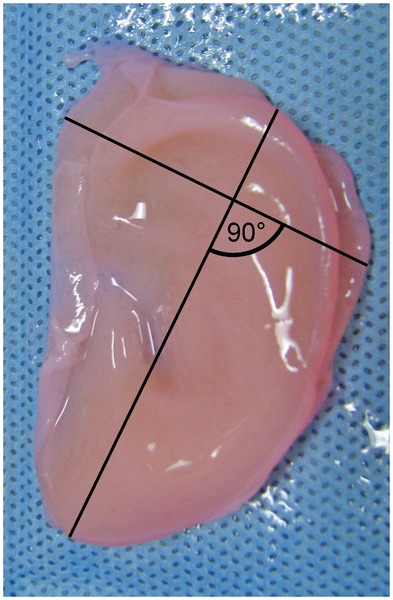
In their PLOS ONE study, the researchers demonstrate how 3D printing and injectable gels made of living cells can be used to fashion ears that are identical to a human ear. Over a three-month period, these flexible ears steadily grew cartilage to replace the collagen that was used to help mould them.
“I believe this will be the novel solution reconstructive surgeons have long wished for to help children born with absence or severe deformity of the ear,” said the study’s co-lead author, Dr Jason Spector, director of the Laboratory for Bioregenerative Medicine and Surgery (LBMS), associate professor of surgery of plastic surgery in the Department of Surgery at Weill Cornell Medical College and an adjunct associate professor in the Department of Biomedical Engineering at Cornell University. “A bioengineered ear replacement like this would also help individuals who have lost part or all of their external ear in an accident or from cancer.”
Currently, replacement ears are constructed using materials that have a Styrofoam-like consistency or, sometimes, surgeons will build ears from rib that is harvested from a young patient. “This surgical option is very challenging and painful for children, and the ears rarely look totally natural or perform well,” said Dr Spector, who is also a plastic and reconstructive surgeon at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. “All other attempts to ‘grow’ ears in the lab - including one 1997 study widely publicised by photos of ears implanted on the backs of mice - have failed in the long term.”
The bioengineered ear is the best to date in appearing and acting like a natural ear, the researchers report. Also, the process of making the ears is fast, taking a week at most.
“This is such a win-win for both medicine and basic science, demonstrating what we can achieve when we work together,” said the study’s other lead author, Dr Lawrence J Bonassar, associate professor and associate chair of the Department of Biomedical Engineering at Cornell University.
Scanning, printing and moulding a human ear in a week
The deformity that both Dr Spector and Dr Bonassar seek to remedy is microtia, a congenital deformity in which the external ear is not fully developed. Although the causes for this disorder are not entirely understood, research has found that microtia can occur in children whose mothers took an acne medication during pregnancy. Typically, only a single ear is affected.
The incidence of microtia varies from almost one to more than four per 10,000 births each year. Many children born with microtia have an intact inner ear but experience hearing loss due to the missing external ear structure, which acts to capture and conduct sound.
Dr Spector and Dr Bonassar have been collaborating on bioengineered human replacement parts since 2007, and Dr Bonassar has also been working with other Weill Cornell physicians. The researchers specifically work to develop replacements for human structures that are primarily made of cartilage, because cartilage does not need to be vascularised with a blood supply in order to survive.
To make the ears, Dr Bonassar and his colleagues first took a combination laser scan and panoramic photo of an ear from twin girls, which provided a digitised 3D image of their ears on a computer screen. That took 30 seconds and did not involve any ionising radiation. The researchers then converted that image into a digitised ‘solid’ ear and used a 3D printer to assemble a mould of the ear. The mould is like a box with a hole in the middle that is in the shape of the mirror image of the ear.
They injected animal-derived collagen - a structural protein frequently used for plastic surgery - into that ear mould, and then added nearly 250 million cartilage cells. The collagen served as a scaffold on which cartilage could grow. The high-density collagen gel, which Cornell researchers developed, resembles the consistency of flexible jelly when the mould is removed.
“The process is fast,” Dr Bonassar said. “It takes half a day to design the mould, a day or so to print it, 30 minutes to inject the gel and we can remove the ear 15 minutes later. We trim the ear and then let it culture for several days in a nourishing cell culture medium before it is implanted.”
During the three-month observation period, the cartilage in the ears grew to replace the collagen scaffold. “Eventually the bioengineered ear contains only auricular cartilage, just like a real ear,” said Dr Spector.
The researchers are now looking at ways to expand populations of human ear cartilage cells in the laboratory so that these cells can be used in the mould.
Dr Spector says the best time to implant a bioengineered ear on a child would be when they are about five or six, when ears are 80% of their adult size. “We don’t know yet if the bioengineered ears would continue to grow to their full size, but I suspect they will,” said Dr Spector. “Surgery to attach the new ear would be straightforward - the malformed ear would be removed and the bioengineered ear would be inserted under a flap of skin at the site.”
Dr Spector says that if all future safety and efficacy tests work out, it might be possible to try the first human implant of the bioengineered ear in as little as three years.
“These bioengineered ears are highly promising because they precisely mirror the native architecture of the human ear,” Dr Spector said. “They should restore hearing and a normal appearance to children and others in need.
“This advance represents a very exciting collaboration between physicians and basic scientists. It is a demonstration of what we hope to do together to improve the lives of these patients with ear deformity, missing ears and beyond.”
Droplet microfluidics for single-cell analysis
Discover how droplet microfluidics is revolutionising single-cell analysis and selection in...
PCR alternative offers diagnostic testing in a handheld device
Researchers have developed a diagnostic platform that uses similar techniques to PCR, but within...
Urine test enables non-invasive bladder cancer detection
Researchers have developed a streamlined and simplified DNA-based urine test to improve early...




