Drug delays tumour growth in models of children's liver cancer
A new drug called WNTinib has been shown to delay the growth of tumours and improve survival in hepatoblastoma, a type of liver cancer that occurs in young children. That’s according to pre-doctoral researcher Ugne Balaseviciute, who presented these findings last month at the 36th EORTC-NCI-AACR Symposium on Molecular Targets and Cancer Therapeutics.
Hepatoblastoma is a rare disease, but is the most frequent liver cancer seen in children under the age of three. There are limited treatment options available — mainly surgery and chemotherapy — and the standard chemotherapy can cause severe and life-long side effects such as hearing loss and heart problems.
“The side effects of chemotherapy can have an especially large impact on children who are treated at an early age,” said Balaseviciute, from the Translational Research in Hepatic Oncology Group led by Professor Josep M Llovet at Barcelona’s Institut D’Investigacions Biomediques August Pi i Sunyer (IDIBAPS). “This highlights the urgent need for new and more effective drugs that are better tolerated by paediatric patients.”
Balaseviciute worked for a year at the Icahn School of Medicine at Mount Sinai, New York, where researchers in collaboration with Llovet had discovered WNTinib — a small molecule that targets a key genetic mutation in hepatoblastoma called CTNNB1, while sparing normal, healthy cells.
“Mutations in the CTNNB1 gene are the most prevalent alteration in hepatoblastoma cells, occurring in about 90% of cases; this suggests that it would be a potential target for drugs that target it,” Balaseviciute said. “However, targeting CTNNB1 mutations is complicated, and no therapies have been approved yet. We wanted to see if WNTinib, which is an effective inhibitor and specifically targets tumours with CTNNB1 mutations, was effective against hepatoblastoma cells and to investigate any mechanisms of resistance to the drug.”
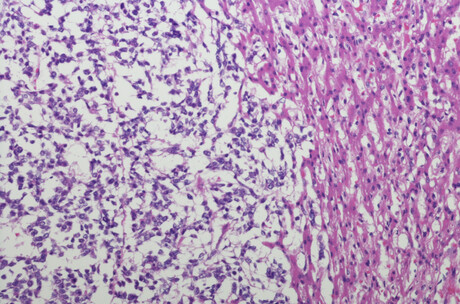
The researchers created three models; they implanted into mice tumour tissue that was either taken from patients, or from two cancer cell lines called HepG2 and TT001 established from patients’ tumours and cultured in the laboratory. The tumours and cancer cells all had CTNNB1 mutations. The mice were treated with WNTinib and the effects were measured against untreated mice or untreated cells.
“Using mice to model the effect of WNTinib on cancer cells can more accurately reflect the outcomes in human patients, as they show how the drug is distributed throughout the body and how the body metabolises it,” Balaseviciute said.
“We observed significantly reduced tumour growth and significantly extended survival by day 21 in mice implanted with patient tumour tissue. Notably, the median survival for the WNTinib-treated group of mice was twice as long, at 42 days, compared to the control group, which had a median survival of 21 days.”
In the second model, in which mice were implanted with the HepG2 cell lines, WNTinib significantly delayed tumour growth compared to the control group. On day 8, treated tumours were 30% smaller than in the control group and 46.5% smaller on day 10. The median (average) survival for the treated mice was 16 days compared to nine days for the control group. The last mouse in the control group lived for 21 days, while (at the time of writing), one mouse in the treatment group was still alive after 148 days.
Similarly, in the model in mice implanted with TT001 cell lines, WNTinib significantly delayed tumour growth. On day 8, treated tumours were 26% smaller than in the control group and 23% smaller on day 10. These mice also survived for longer; 45% of them lived longer than 30 days and three mice were still alive after 106, 118 and 127 days, compared to the control arm where none survived beyond 20 days.
“Notably, tumours shrank in 45% of the TT001 animals treated with WNTinib and, of these, the tumours disappeared completely in 80% of them,” Balaseviciute said.
“Overall, in all three preclinical models, we observed effective inhibition of tumour growth and a significant improvement in overall survival in hepatoblastoma with the CTNNB1 mutation. These findings suggest a promising new treatment strategy that could enhance survival in children with hepatoblastoma who carry CTNNB1 mutations. However, further studies into how WNTinib works are necessary.
“The long-term goal is to improve the efficacy and reduce general toxicity through the use of drugs such as WNTinib for the treatment of CTNNB1-mutant hepatoblastoma tumours.”
The researchers also screened enzymes (or proteins), called kinases, involved in cellular processes. Out of 763 human kinase genes, they identified several that played a potential role in cancer’s response to WNTinib and in the mechanisms of resistance to the drug. They are now evaluating some of the top ones, such as DYRK1A, PRKC1 and CDK14, to see if they could be targets for WNTinib treatment together with another drug.
“We have identified the protein, DYRK1A, whose inhibition may enhance the efficacy of WNTinib,” Balaseviciute said. “Preliminary data in cell lines indicate that low concentrations of this inhibitor can increase sensitivity to WNTinib. However, more research needs to be carried out to validate these findings.”
Balaseviciute concluded: “Understanding WNTinib’s mechanisms and effectiveness in liver cancer can open the door to exploring its potential in other cancers that harbour CTNNB1 mutations. This could have an impact on clinical guidelines and the management of hepatoblastoma patients. It could also enhance treatment outcomes for patients with less adverse effects and advance precision medicine for treating cancer.”
'Woolly mouse' created on the quest to bring back the mammoth
By modifying seven genes simultaneously, Colossal created mice with a coat colour, texture and...
Biotherapeutics: what do we make next?
Two recent AI methods, RFdiffusion and ProteinMPNN, have totally changed the nature of...
Targeted therapy for childhood brain cancer shows promise
A potential new targeted therapy for childhood brain cancer is effective in infiltrating and...




