Funding a cure for type 1 diabetes
Doctors and scientists based at the Westmead Millennium Institute for Medical Research and Westmead Hospital have been awarded $3.3 million to extend their research into a clinical cure for type 1 diabetes — a chronic autoimmune disease affecting 120,000 Australians.
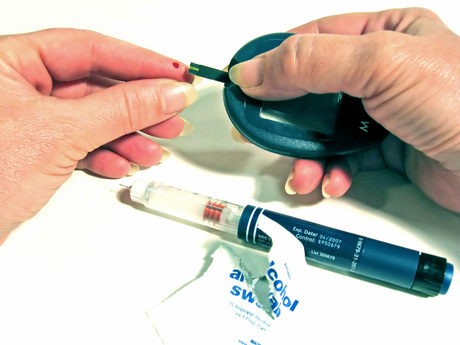
Type 1 diabetes destroys the body’s insulin-producing cells, which normally prevent blood-sugar levels from becoming dangerously high. As noted by Professor Philip O’Connell, the leader of the Westmead research, “Until now, treatment has focused on managing the consequences and complications of type 1 diabetes.”
Professor O’Connell and his team have sought to change this, taking insulin-producing islet cells from a donor pancreas and infusing them into the liver of a patient with type 1 diabetes via the portal vein. There, the islet cells populate and start producing insulin, providing a practical cure for an otherwise debilitating disease.
Professor O’Connell said clinical trials underway at Westmead Hospital and elsewhere since 2006 have proven the technique to be highly successful. But so far its use has been limited to a small number of patients with so-called ‘brittle’ diabetes.
“The current need for transplant recipients to take powerful drugs for the rest of their lives to prevent islet rejection means the technique has been reserved for people with life-threatening undetected hypoglycaemia and is not suitable for children or younger patients,” he said.
Now, the Type 1 Diabetes Clinical Research Network (T1DCRN) has awarded Professor O’Connell’s team a grant to advance this research. The network’s funding is designed to plug the gap between lab-based research and expensive clinical trials that prevents new type 1 diabetes treatments entering widespread use.
“Winning a grant of this size allows us to assemble the necessary expertise to develop a completely new therapeutic paradigm, which not only has the potential to improve islet transplantation but will also have the potential to treat the disease before diabetes has manifested,” Professor O’Connell said.
“It will allow us to concentrate on prevention and cure — so that one day, patients won’t need insulin injections or pumps, and medical complications will be a thing of the past.”
The four-year research program will aim to develop alternative strategies that promote immune tolerance towards transplanted pancreatic islets, thereby making islet transplantation a viable option for a wider range of Australians living with type 1 diabetes.
“The average age of patients when they suffer the onset of type 1 diabetes is just 11 years, so if we could successfully use pancreatic islet transplantation in the young, it would solve a significant problem,” Professor O’Connell said. He added that the research could bring his team closer to “achieving the goal of drug-free immunosuppression, which may benefit the recipients of other types of transplants”.
AI-designed DNA switches flip genes on and off
The work creates the opportunity to turn the expression of a gene up or down in just one tissue...
Drug delays tumour growth in models of children's liver cancer
A new drug has been shown to delay the growth of tumours and improve survival in hepatoblastoma,...
Ancient DNA rewrites the stories of those preserved at Pompeii
Researchers have used ancient DNA to challenge long-held assumptions about the inhabitants of...




