Synthetic peptide takes away bacteria's drug resistance
Scientists at Nanyang Technological University, Singapore (NTU Singapore) have developed a synthetic peptide that can make multidrug-resistant bacteria sensitive to antibiotics again when used together with traditional antibiotics, offering hope for the prospect of a combination treatment strategy to tackle certain antibiotic-tolerant infections. The synthetic antimicrobial peptide can also kill bacteria that have grown resistant to antibiotics.
Antibiotic resistance arises in bacteria when they can recognise and prevent drugs that would otherwise kill them from passing through their cell wall. This threat is accelerated by the developing COVID-19 pandemic, with patients admitted to hospitals often receiving antibiotics to keep secondary bacterial infections in check, amplifying the opportunity for resistant pathogens to emerge and spread.
“While efforts are focused on dealing with the COVID-19 pandemic, we should also remember that antibiotic resistance continues to be a growing problem, where secondary bacterial infections that develop in patients could complicate matters, posing a threat in the healthcare settings,” said Professor Mary Chan, Director of NTU’s Centre of Antimicrobial Bioengineering. “For instance, viral respiratory infections could allow bacteria to enter the lungs more easily, leading to bacterial pneumonia, which is commonly associated with COVID-19.”
Antimicrobial peptides, which carry a positive electric charge, typically work by binding to the negatively charged bacterial membranes, disrupting the membrane and causing the bacteria to die eventually. The more positively charged a peptide is, the more efficient it is in binding to bacteria and thus killing them. However, the peptide’s toxicity to the host also increases in line with the peptide’s positive charge — it damages the host organism’s cells as it kills bacteria. As a result, engineered antimicrobial peptides to date have met with limited success.
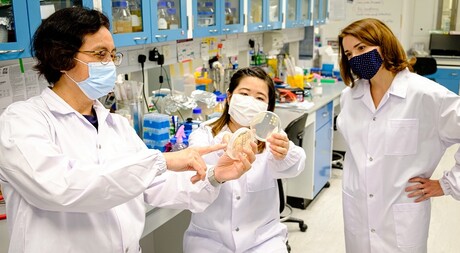
The NTU Singapore team, led by Prof Chan and Associate Professor Kimberly Kline, developed an antimicrobial peptide known as CSM5-K5 comprising repeated units of chitosan — a sugar found in crustacean shells that bears structural resemblance to the bacterial cell wall — and repeated units of the amino acid lysine. The scientists believe that chitosan’s structural similarity to the bacterial cell wall helps the peptide interact with and embed itself in it, causing defects in the wall and membrane that eventually kill the bacteria.
CSM5-K5 is able to cluster together to form nanoparticles when it is applied to bacteria biofilms, which can cling onto surfaces (including living tissues) and are difficult for traditional antibiotics to penetrate. This clustering results in a more concentrated disruptive effect on the bacterial cell wall when compared to the activity of single chains of peptides, meaning it has high antibacterial activity but without causing undue damage to healthy cells.
To examine CSM5-K5’s efficacy on its own, the scientists developed separate biofilms comprising methicillin-resistant Staphylococcus aureus (MRSA), a highly virulent multidrug-resistant strain of Escherichia coli (MDR E. coli) and vancomycin-resistant Enterococcus faecalis (VRE), the latter two of which are classified as serious threats by the US Centers for Disease Control and Prevention. In lab experiments, CSM5-K5 killed more than 99% of the biofilm bacteria after four hours of treatment; in infected wounds on mice, the peptide killed more than 90% of the bacteria.
When CSM5-K5 was used with conventional antibiotics, the NTU team found that the combination approach led to a further reduction in the bacteria in both lab-formed biofilms and infected wounds in mice as compared to when only CSM5-K5 was used, suggesting that the antimicrobial peptide made the bacteria sensitive to the drugs they would otherwise be resistant to. The team also found that the three strains of bacteria studied developed little to no resistance against CSM5-K5 and, while MRSA developed low-level resistance against CSM5-K5, this made MRSA more sensitive to the drug it is otherwise resistant to. The amount of antibiotics used in this combination therapy was also at a concentration lower than what is commonly prescribed.
“Our findings show that our antimicrobial peptide is effective whether used alone or in combination with conventional antibiotics to fight multidrug-resistant bacteria,” Assoc Prof Kline said. “Its potency increases when used with antibiotics, restoring the bacteria’s sensitivity to drugs again. More importantly, we found that the bacteria we tested developed little to no resistance against our peptide, making it an effective and feasible addition to antibiotics as a viable combination treatment strategy as the world grapples with rising antibiotic resistance.”
“Developing new drugs alone is no longer sufficient to fight difficult-to-treat bacterial infections, as bacteria continue to evolve and outsmart antibiotics,” Prof Chan added. “It is important to look at innovative ways to tackle difficult-to-treat bacterial infections associated with antibiotic resistance and biofilms, such as tackling the bacteria’s defence mechanisms. A more effective and economic method to fight bacteria is through a combination therapy approach like ours.”
The team’s findings have been published in the journal ACS Infectious Diseases. Their next step is to explore how a combination therapy approach can be used for rare diseases or for wound dressing.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...
Clogged 'drains' in the brain an early sign of Alzheimer’s
'Drains' in the brain, responsible for clearing toxic waste in the organ, tend to get...
World's oldest known RNA extracted from woolly mammoth
The RNA sequences are understood to be the oldest ever recovered, coming from mammoth tissue...





