Stamping out invasive biopsies
Researchers from the National University of Singapore (NUS) have developed a novel technology that could sensitively and accurately detect and classify cancer cells, as well as determine disease aggressiveness, from the least invasive biopsies.
Known as STAMP (Sequence-Topology Assembly for Multiplexed Profiling), the technology could enable comprehensive disease information to be obtained faster, at a much earlier stage of the clinical workflow, allowing doctors to decide and administer treatments earlier and more effectively. It was developed by researchers at the NUS Institute for Health Innovation & Technology (NUS iHealthtech) over more than two years, and has now been described in the journal Nature Biomedical Engineering.
A biopsy, which involves removing a small amount of tissue from the body, is the main way for doctors to diagnose most cancers. While less invasive biopsy procedures are preferred, they can yield insufficient samples, resulting in incomplete and/or inconclusive diagnosis. A definitive diagnosis and further analysis such as cancer staging can only be made post-surgery; this long-waited information is then used to guide subsequent treatment decisions.
Comprehensive analysis of protein expression and distribution meanwhile holds great promise for discovery of biomarkers, early disease detection and rationalising of treatment options. However, current approaches involve imaging and microscopy techniques, which are complex, time-consuming and have a limited multiplexing capability. STAMP was conceptualised and developed to address these many challenges, measuring billions of protein markers from a small clinical sample and revealing important clinical information which currently can only be obtained through post-surgery tissue analysis — all directly from a fine needle aspiration (FNA) biopsy, the least invasive form of biopsy.
DNA exists in nature as long ‘ribbons’ to store massive genetic information through its combination of base codes, but it can also be precisely engineered to fold into 3D nanostructures with enhanced stability. STAMP leverages these two important properties of DNA — a large capacity to store information as well as its programmability to fold and unfold into different structures — to engineer convertible barcodes. These STAMP barcodes can be used to measure billions of protein markers in a single test and identify the specific locations of these protein markers in cells.
“To label diverse protein markers in cells, STAMP uses DNA barcodes which are folded as compact nanostructures,” said Noah Sundah, a doctoral student from NUS iHealthtech and first author of the study. “These 3D barcodes achieve a high labelling efficiency and remain stable against biological degradation. Each 3D barcode is further given a localisation label to encode protein marker location and distribution within the cell.
“To perform analysis, these 3D barcodes are unfolded on demand through heating to release a pool of linear DNA, which can be easily analysed using established technologies such as PCR and DNA sequencing. In this way, the expression of a very large number of protein markers and their distribution in cells can be sensitively measured in a single test.”
Assistant Professor Shao Huilin, who led the NUS iHealthtech team, added, “By mapping these marker distribution patterns in cells, STAMP can provide an early indication of disease aggressiveness. Current pathology techniques only measure a small subset of protein markers and require several days of extensive processing. In comparison, STAMP is a million times more sensitive, provides highly informative analysis from scarce samples and can be completed in as little as two hours.”
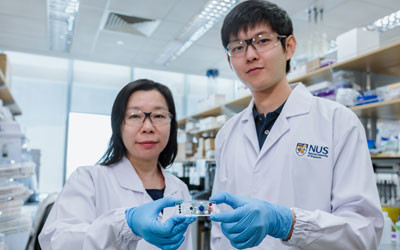
To facilitate clinical processing and measurement, the research team implemented the STAMP technology on a small microfluidic chip that is about half the size of a credit card. Test results could be generated from small amounts of clinical samples, and each test is estimated to cost around $50.
To validate STAMP’s performance, the research team conducted a clinical study involving 69 breast cancer patients. FNA biopsies were collected from each patient and analysed using STAMP. For comparison, gold-standard pathology analysis was performed on post-surgery tissues for all patients.
The STAMP analysis of the FNA samples demonstrated a high level of accuracy of more than 94% for cancer diagnosis and subtyping, making it equally accurate as pathology analysis of surgical tissues. Importantly, based on its comprehensive protein marker analysis, STAMP was also able to accurately identify disease aggressiveness from the scarce biopsy samples.
Asst Prof Shao and her team are currently in discussions with industry partners to further develop and commercialise STAMP; a provisional patent has been filed and the technology is expected to reach the market within the next five years. Moving forward, the research team hopes to expand the applications of STAMP to other types of cancer, such as brain, lung and gastric cancer, as well as validate the technology in other samples, such as blood and ascites.
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Mast cell test simplifies the diagnosis of food allergies
In the Hoxb8 mast cell activation test (Hoxb8 MAT), mast cells grown in the laboratory are...
A science-based solution for tackling lake health
Experts urge moving away from short-term 'fixes' that only worsen a lake's condition...
Climate report warns of perilous times ahead
Scientists have warned that the Earth is stepping into a critical and unpredictable new phase of...




